Rapid Search Terms
- Anatomy
- Medical Overview
- Smoking
- Diabetics
- Osteoporosis and/or Bisphosphonates
- Radiation Therapy
- Other Disorders involving Bone
- Anticoagulants
- Other medications
- Periodontal disease
- Parafunction and Overloading
- Age at Placement (growth)
- Age at placement (outcome)
Study Questions
Basic overview of anatomy / Anatomy and Surgical Significance
- Please describe the blood supply to the maxilla.
- What clinical findings may be a cause for concern with the sinus? (Dutolt-2003, Root impaction, Sinusitis, OA fistula, Periapical abscess, odontogenic cyst, Fractures, Polyps, tumors.)
- Describe the position of greater palatine foramen. (Chrcanovic 2011- 54.7% of GPF were opposite to maxillary 3rd molar, 38.9% distal to maxillary 3rd molar, and 6.19% between maxillary 2nd and 3rd molars.)
- Describe the morphology of the mandibular lingual ridge. (Nilsun-2019, results show that class I patients- edentulous on both sides, had the maximum concavity depth and higher measurements than the other types. In class II- one site is edentulous and the other is dentate, a significant difference was found between the left and right sides. male patients’ dimensions and pts35 years old had deeper concavities. Galluci-201, The ridge shape significantly influenced the ease or difficulty of placing an implant. The s-shape- 7.4%, hourglass-1.9%, and basal bone- 10.8% posterior mandibular cross-sectional shapes were associated with a higher degree of difficulty. Straight-53.6 and Oblque-26.2% incidences were more straightforward for DI placement.)
- What treatment considerations must be considered in the case of a mandibular lingual cortical plate perforation? (Mardinger-2007, perimandibular blood vessels. Kalpedis-2004, – Implant placement may induce lingual perforations in the inclined atrophic edentulous mandible & severe hemorrhage. Worst area was canine.)
Medical History: systemic conditions + drugs that may affect implant and surgical outcome
- Which medical risk factors may have a negative effect on osseointegration? (Aghaloo-2019, smoking, diabetes, osteoporosis / bisphosphonates, radiation therapy, Anticoagulants, SSRIs, PPIs, antihypertensives, age, periodontal disease, and parafunctional habits. Clemintini-2014, However the level of evidence is high only for smoking).
- What is the approximate failure rate of DIs in smokers vs non-smokers? (Chrcanovich-2014, 35% vs 3.18%, or 2.23x greater, Al-Aali 2018- Probing depth of >=4 mm, Peri-implant bone loss, and TNF-a and IL-1b levels were significantly higher Vaping patients. Moraschini 2015- marginal bone loss was significantly higher in smokers. maxillary arch revealed higher levels of resorptions when compared to the mandible and implant failure rate was found to be significantly higher in smokers.)
- Do diabetic patients with dental implants have greater complication rates and lower survival rates compared to non-diabetics? (Naujokat-2016, Patients with poorly controlled diabetes have impaired osseointegration, elevated risk of peri-implantitis, and higher level of implant failure when observed over 20 years, while little difference was seen in 6 years. Monje-2017, The risk of peri-implantitis in hyperglycemia is between 1.21 and 2.46 fold statistically significantly higher than in normoglycemia.)
- What is the effect of antiresorptive drugs like bisphosphonates on implant therapy? (Stavropoulos-2019, NSSD were observed in terms of implant loss with low-dose oral bisphosphonate intake between cases and controls in reviewed studies. Not enough information was available on high dose regimens. Kwon 2014- Oral BP users were most common (79%) compared with IV BP. Alendronate was the most commonly related drug. 58% pts developed BRONJ w/o any relation to surgical trauma from insertion or removal of the dental implant. Stavropoulos 2018- MRONJ Associated with Implants- IV bisphosphonates were present in 61 cases, and oral in 44 cases. Hormone Replacement Therapy: Higher implant loss rate 9.1%-27.3% compared to controls, a relative risk of 2.55).
- How might radiation therapy affect the implant patient? (Claudy 2013- Patients undergoing radiation will benefit more waiting 1-year post radiation treatment. 588 implants were placed between 6- 12months and 920 implants were placed after 12 months post-radiation 80 implants failed resulting in a 13.6% failure rate. Curi 2018- Patients treated with IMRT had an implant success rate of 96.1%. No significant difference was observed in implants placed in maxilla or mandible. Patients receiving HBOT also showed no significant difference in implant success.)
- How would your approach change if your target area for implant therapy had Florid Cemento-Osseous Dysplasia? (Gerlach 2013- elective surgical procedures that include extractions, periodontal surgery, oral surgery, and implant therapy, are contraindicated. Decrease in bone vitality and resultant of calcifications, decreased vascularity, thereby reducing the capacity of osseous regeneration, osseointegration, and healing.)
- How might periodontitis effect the degree of implant success? (Swierkot-2012– Implant survival rate of 100% in periodontally healthy patients vs. 96% in Gen AgP patients. Implant success rate was 33% in Gen AgP vs. 50% in periodontally healthy patients. Zagrando 2015- Implant therapy is successful in patients with a diagnosis of periodontitis, as long as the periodontitis is properly treated and pt has maint. 10yr success = 92%. Rasperini-2013. Arunyanak-2019)
- Do patients exhibiting parafunctional habits experience more implant complications? If so, what types of complications? (Chitumalla 2018- Survival rate of dental implants with bruxism habit was 90%-92% after 1 year, 87%-90% after 2 years, 85% after 3 years, 75% after 4 years, and 70-72% after 5 years. Common complications were fracture of implant, fracture of ceramic/porcelain, screw loosening, screw fracture, and decementation. Chrcanovich 2015- Meta. Placement of dental implants in bruxers affected implant failure rates, a relative risk of 2.93 was found. The insertion of implants in bruxers increases the risk of implant failure by 193% compared to non-bruxers.)
References:
Anatomy and Radiology
- Al-Rawee RY, Abdalfattah MM (2020) Anatomy Respect in Implant Dentistry. Assortment, Location, Clinical Importance (Review Article). J Dent Probl Solut 7(2): 068-078.
- Greenstein, G., & Tarnow, D. (2006). The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. Journal of Periodontology, 77(12), 1933–1943
- Neiva RF, Gapski R, et al. Morphometric analysis of implant related anatomy in Caucasian skulls. J Periodontol 2004; 75(8): 1061-1067
- Du Tolt DF, Nortje C. The maxillae: integrated and applied anatomy relevant to dentistry. SADJ 2003; 58(8):325-330.
- Chrcanovic BR, Abreu MH, Custódio AL. A morphometric analysis of supraorbital and infraorbital foramina relative to surgical landmarks. Surg Radiol Anat. 2011 May;33(4):329-35.
- Chrcanovic BR, Custódio AL. Anatomical variation in the position of the greater palatine foramen. J Oral Sci. 2010 Mar;52(1):109-13.
- Galluci GO et al. Influence of the Posterior Mandible Ridge Morphology on Virtual Implant Planning. Int J Oral Maxillafac Implants 2017 Jul/Aug; 32(4): 801-806
- Urban IA, et al. Mandibular Regional Anatomical Landmarks and Clinical Implications for Ridge Augmentation. Int J Periodontics Restorative Dent. 2017 May/Jun;37(3):347-353.
- Quirynen M, Mraiwa N, et al. Morphology and dimensions of the mandibular jaw bone in the interforaminal region in patients requiring implants in the distal areas. Clin Oral Implants Res. 2003 Jun;14(3):280-5.
- Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol. 2004 May;75(5):631-45
- Mardinger O et al: Lingual perimandibular vessels associated with life – threatening bleeding. An anatomic study. Int J Oral Maxillofac Implants 2007; 22:127-131
- Nilsun B et al. Cone-Beam Computed Tomography Evaluation of the Submandibular Fossa in a group of dental implant patients. Implant Dent 2019 Aug;28(4):329-339.
- Al-Ekrish AA. Radiology of Implant Dentistry. Radiol Clin North Am. 2018 Jan;56(1):141-156.
- Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusinanag on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants. 2014;29 Suppl:55-77.
- Jacobs R, Salmon B, Codari M, Hassan B, Bornstein MM. Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health. 2018 May 15;18(1):88.
- Rios HF, Borgnakke WS, Benavides E. The Use of Cone-Beam Computed Tomography in Management of Patients Requiring Dental Implants: An American Academy of Periodontology Best Evidence Review. J Periodontol. 2017 Oct;88(10):946-959.
- Iwanaga J, Katafuchi M, Matsushita Y, Kato T, Horner K, Tubbs RS. Anatomy of the mandibular canal and surrounding structures: Part I: Morphology of the superior wall of the mandibular canal. Ann Anat . 2020 Nov;232:151580.
- Mishra SK, Nahar R, Gaddale R, Chowdhary R. Identification of anterior loop in different populations to avoid nerve injury during surgical procedures-a systematic review and meta-analysis. Oral Maxillofac Surg. 2021 Jun;25(2):159-174.
- Schriber M, Yeung AWK, Suter VGA, Buser D, Leung YY, Bornstein MM. Cone beam computed tomography artefacts around dental implants with different materials influencing the detection of peri-implant bone defects. Clin Oral Implants Res. 2020 Jul;31(7):595-606.
- Wada M, Tsuiki Y, Suganami T, Ikebe K, Sogo M, Okuno I, Maeda Y. The relationship between the bone characters obtained by CBCT and primary stability of the implants. Int J Implant Dent. 2015 Dec;1(1):3
- de Elío Oliveros J, Del Canto Díaz A, Del Canto Díaz M, Orea CJ, Del Canto Pingarrón M, Calvo JS. Alveolar Bone Density and Width Affect Primary Implant Stability. J Oral Implantol. 2020 Aug 1;46(4):389-395.
Medical Overview
- Carr AB, Revuru VS, Lohse CM. Association of Systemic Conditions with Dental Implant Failures in 6,384 Patients During a 31-Year Follow-up Period. Int J Oral Maxillofac Implants. 2017 Sept/Oct;32(5):1153-1161
- Clementi M et al. Systemic risk factors for peri-implant bone loss: a systematic review and meta-analysis. Int J Oral Maxillofac Surgery. 2014; 43:323-334.
- Sugerman, P., Barber, M.: Patient selection for endossous dental implants; Oral and systemic considerations. Int J Oral Maxillofac Implants. 2002 Mar-Apr; 17(2):191-201
Smoking as a risk factor for implant failure
- Klokkevold P, Han T: How do smoking, diabetes and periodontits affect outcomes of implant treatment? Int J Oral Maxillofac Implants. 2007; 22 (suppl)173-202
- Strietzel FP, Reichart PA, et al. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol. 2007 Jun;34(6):523-44. Review.
- Moraschini V, Barboza ED. Success of dental implants in smokers and non-smokers: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2015 Sep 15.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: A systematic review and meta-analysis. J Dent. 2015 May;43(5):487-498
- Bain CA, et al. Implant installation in the smoking patient. Periodontol 2000. 2003;33:185-93.
- Naseri R, Yaghini J, Feizi A. Levels of smoking and dental implants failure: A systematic review and meta-analysis. J Clin Periodontol. 2020 Apr;47(4):518-528
- Javed F, Rahman I, Romanos GE. Tobacco-product usage as a risk factor for dental implants. Periodontol 2000. 2019 Oct;81(1):48-56.
Diabetics
- Nobre Mde A, Maló P, Gonçalves Y, Sabas A, Salvado F. Outcome of dental implants in diabetic patients with and without cardiovascular disease: A 5-year post-loading retrospective study. Eur J Oral Implantol. 2016 Spring;9(1):87-95.
- Naujokat H, Kunzendorf B, Wiltfang J. Dental Implants and diabetes mellitus-a systematic review. Int J Implant Dent. 2016 Dec;2(1):5
- Monje A, Catena A, Borngakke WS. Association between diabetes mellitus/hyperglycemia and peri-implant disease: systematic review and meta-analysis. J Clin Periodontol. 2017 Jun;44(6):636648.
Osteoporosis and/or Bisphosphonates
- Holahan, C et al: Effect of osteoporotic status on the survival of titanium dental implants. Int J Oral Maxillofac Implants. 2008:Sep-Oct; 23(5)905-10
- Temmerman A, et al. A Prospective, Controlled, Multicenter Study to Evaluate the Clinical Outcome of Implant Treatment in Women with Osteoporosis/Osteopenia: 5 year results. J Dent Res. 2019 Jan;98(1):84-90.
- Kwon TG et al. Osteonecrosis associated with dental implants in patients undergoing bisphosphonate treatment. Clin Oral Implants Res. 2014 May;25(5):632-640
- Stavropoulos A, et al. The effect of antiresorptive drugs on implant therapy: systematic review and meta-analysis. Clin Oral Implants Res. 2018 Oct;29 suppl 18:54-92.
- Ata-Ali J, Ata-Ali F, Peñarrocha-Oltra D, Galindo-Moreno P. What is the impact of bisphosphonate therapy upon dental implant survival? A systematic review and meta-analysis. Clin Oral Implants Res. 2016 Feb;27(2):e38-46.
Radiation Therapy
- Colella, Cannavale, Pentenero, Gandolfo: Oral implants in radiated patients: A systematic review. Int J Orla Maxillofac Implants 2007; 22(4):616-623
- Claudy MP, Miguens SA Jr, et al Time Interval after Radiotherapy and Dental Implant Failure: Systematic Review of Observational Studies and Meta-Analysis. Clin Implant Dent Relat Res. 2013 Jun 7. [Epub ahead of print]
- Atanásio Pitorro TE, Survival of Dental Implants Placed Pre-Radiotherapy Versus Post-Radiotherapy in Native Bone: A Systematic Review. Int J Oral Maxillofac Implants. 2022 Nov-Dec;37(6):1100-1109. doi: 10.11607/jomi.9756. PMID: 36450015.
Other disorders involving bone or soft tissue
- Gerlach RC et al. Case presentation of florid cemento-osseous dysplasia with concomitant cemento-ossifying fibroma discovered during implant explantation. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013 Mar;115(3): e44-52
- Friberg B. Brånemark System Implants and Rare Disorders: A Report of Six Cases. Int J Perio Rest Dent 2013; (33):139-48.
- Strietzel FP, et al. Implants in patients with oral manifestations of autoimmune of mucocutaneous diseases-a systematic review. Med Oral Patol Cir Bucal 2019 Mar 1;24(2):e217-30.
Anticoagulants
- Madrid C, Sanz M. What influence do anticoagulants have on oral implant therapy? A systemic review. Clin Oral Impl Res (Suppl 4) 2009; 10: 96-106.
- Broekema FI, et al. Risk of bleeding after dentoalveolar surgery in patients taking anticoagulants. Br J Oral Maxillofac Implants 2014; 52:e15-e19.
- Gomez-Morena G, et al. Dental implant surgery in patients in treatment with the anticoagulant oral rivaroxaban. Clin Oral Imp Res. 2016; 27:730-733
Other Medications Issues:
- Chrcanovic BR et al. Intake of Proton Pump Inhibitors is Associated with an Increased Risk of Dental Implant Failure. Int J Oral Maxillofac Implants 2017 Sept/Oct;32(5): 1097-1102.
- Wu X, Al-Abedalla K, Abi-Nader S, Daniel NG, Nicolau B, Tamimi F. Proton Pump Inhibitors and the Risk of Osseointegrated Dental Implant Failure: A Cohort Study. Clin Implant Dent Relat Res. 2017 Apr;19(2):222-232.
- Chrcanovic BR et al. Is the intake of selective serotonin reuptake inhibitors associated with an increased risk of dental implant failure? Int J Oral Maxillofac Surg. 2017 June;46(6):782-788
- Chappius V, et al. Medication-related dental implant failure: systematic review and meta-analysis. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:55-68.
- Radzewski R, Osmola K. Osseointegration of Dental Implants in organ transplant patients undergoing chronic immunosuppressive therapy. Implant Dent. 2019 Jul 12 epub ahead of print
- Zahra B, Nicholas B, Geoffrey R, Dina Z, Janal MN, Stuart F. Dental implant failure rates in patients with self-reported allergy to penicillin. Clin Implant Dent Relat Res. 2022 Jun;24(3):301-306.
- Carr AB, Revuru VS, Lohse CM. Risk of Dental Implant Failure Associated With Medication Use. J Prosthodont. 2019 Aug;28(7):743-749.
- Carr AB, Gonzalez RLV, Jia L, Lohse CM. Relationship between Selective Serotonin Reuptake Inhibitors and Risk of Dental Implant Failure. J Prosthodont. 2019 Mar;28(3):252-257.
Periodontal disease as a risk factor for implant failure
- Guarnieri R, Di Nardo D, Di Giorgio G, Miccoli G, Testarelli L. Longevity of Teeth and Dental Implants in Patients Treated for Chronic Periodontitis Following Periodontal Maintenance Therapy in a Private Specialist Practice: A Retrospective Study with a 10-Year Follow-up. Int J Periodontics Restorative Dent. 2021 Jan-Feb;41(1):89-98.
- Safii SH, Palmer RM, Wilson RF. Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: a systematic review and meta-analysis. Clin Implant Dent Relat Res. 2010 Sep;12(3):165-74.
- Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res. 2015 Apr;26(4):e8-e16.
- Sousa V, Mardas N, Farias B, Petrie A, Needleman I, Spratt D, Donos N. A systematic review of implant outcomes in treated periodontitis patients. Clin Oral Implants Res. 2016 Jul;27(7):787-844.
- Quirynen M, Abarca M, Van Assche N, Nevins M, van Steenberghe D. Impact of supportive periodontal therapy and implant surface roughness on implant outcome in patients with a history of periodontitis. J Clin Periodontol. 2007 Sep;34(9):805-15.
- Levin L, Ofec R, Grossmann Y, Anner R. Periodontal disease as a risk for dental implant failure over time: a long-term historical cohort study. J Clin Periodontol. 2011 Aug;38(8):732-7.
- Carra MC, Rangé H, Swerts PJ, Tuand K, Vandamme K, Bouchard P. Effectiveness of implant-supported fixed partial denture in patients with history of periodontitis: A systematic review and meta-analysis. J Clin Periodontol. 2022 Jun;49 Suppl 24:208-223.
- Roccuzzo A, Imber JC, Marruganti C, Salvi GE, Ramieri G, Roccuzzo M. Clinical outcomes of dental implants in patients with and without history of periodontitis: A 20-year prospective study. J Clin Periodontol. 2022 Dec;49(12):1346-1356.
- Monje A, Alcoforado G, Padial-Molina M, Suarez F, Lin GH, Wang HL. Generalized aggressive periodontitis as a risk factor for dental implant failure: a systematic review and meta-analysis. J Periodontol. 2014 Oct;85(10):1398-407.
- Smith MM, Knight ET, Al-Harthi L, Leichter JW. Chronic periodontitis and implant dentistry. Periodontol 2000. 2017 Jun;74(1):63-73.
Parafunction and Overloading
- Chitumalla R, et al. Assessment of Survival Rate of Dental Implants in patients with bruxism: a 5 year retrospective study. Contemp Clin Dent. 2018 Sept;9(suppl 2):S278-S282.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Bruxism and Dental Implants: A Meta-Analysis. Implant Dent. 2015 Oct;24(5):505-16
- Bertolini MM, Del Bel Cury AA, Pizzoloto L, Acapa IRH, Shibli JA, Bordin D. Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review. Braz Oral Res. 2019 Sep 30;33(suppl 1):e069.
- Nagasawa M, Takano R, Maeda T, Uoshima K. Observation of the bone surrounding an overloaded implant in a novel rat model. Int J Oral Maxillofac Implants. 2013 Jan-Feb;28(1):109-16.
- Zhou Y, Gao J, Luo L, Wang Y. Does Bruxism Contribute to Dental Implant Failure? A Systematic Review and Meta-Analysis. Clin Implant Dent Relat Res. 2016 Apr;18(2):410-20.
- Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005 Feb;16(1):26-35.
- Naert I, Duyck J, Vandamme K. Occlusal overload and bone/implant loss. Clin Oral Implants Res. 2012 Oct;23 Suppl 6:95-107.
- Chambrone L, Chambrone LA, Lima LA. Effects of occlusal overload on peri-implant tissue health: a systematic review of animal-model studies. J Periodontol. 2010 Oct;81(10):1367-78.
- Goldstein G, Goodacre C, Taylor T. Occlusal Schemes for Implant Restorations: Best Evidence Consensus Statement. J Prosthodont. 2021 Apr;30
Age at Placement (growth)
- Cronin RJ Jr, Oesterle LJ. Implant use in growing patients. Treatment planning concerns. Dent Clin North Am 1998;42(1):1-34.
- Mankani N et al. Osseointegrated dental implants in growing children: a literature review. J Oral Implantol 2014. Oct;40(5):627-31.
- Heijl D eta al: Facial development, continuous tooth eruption and mesial drift as compromisisng factors for implant placement. Int J Ora Maxillofac Implants. 2006 Nov-Dec; 21(6)867-78
- Fudalej P., Kokich V., Leroux B: Determing the cessation of vertical growth of the craniofacial structures to facilitate placement of single-tooth implants. Am J Orthod Dentofacial Orthop. 2007 Apr; 131 (4 Suppl):S59-67
- Oesterle LJ, Cronin RJ Jr. Adult growth, aging, and the single-tooth implant. Int J Oral Maxillofac Implants 2000;15(2):252-260.
- Schwartz-Arad D, Bichacho N. Effect of Age on Single Implant Submersion Rate in the Central Maxillary Incisor Region: A Long-Term Retrospective Study. Clin Implant Dent Relat Res. 2015 Jun;17(3):509-514.
Age at placement (outcome)
- Chvartszaid D, et al. Thematic Abstract Review: Implants and the Spectrum of Aging. Int J Oral Maxillofac Implants 2017 Sep/Oct;32(5):965-968
- Hoeksema AR, Visser A, Raghoebar GM, Vissink A, Meijer HJ. Influence of Age on Clinical Performance of Mandibular Two-Implant Overdentures: A 10-Year Prospective Comparative Study. Clin Implant Dent Relat Res. 2016 Aug;18(4):745-51.
- Becker W, Hujoel P, Becker BE, Wohrle P. Dental Implants in an Aged Population: Evaluation of Periodontal Health, Bone Loss, Implant Survival, and Quality of Life. Clin Implant Dent Relat Res. 2015 Jun 17.
- Schimmel M, et al. Effect of advanced age and/or systemic medical conditions on dental implant survival: a systematic review and meta-analysis. Clin Oral Implants Res. 2018 Oct;29 suppl 16:311330.
Medical Overview
Topic: Medical Overview
Title Association of Systemic Conditions with Dental Implant Failures in 6,384 Patients During a 31-Year Follow-up Period.
Source: Int J Oral Maxillofac Implants. 2017 Sept/Oct;32(5):1153-1161
DOI:
Type: Retrospective Cohort Study
Keywords: association, implant failure, patient-based, systemic condition, systemic disease
Purpose: identify associations between implant failure and system conditions or disease in a consecutive series of patients who received dental implants from October1, 1983, to December 31, 2014, in the Department of Dental Specialties at Mayo Clinic in Rochester, Minnesota.
Methods: Data were imported from a prospective clinical database and electronic health records for patients’ demographic, implant-specific, and medical profiles to deterimine time to first implant failure. Survival free of implant failure at the patient level was estimated using the Kaplan-Meier method. Association of demographic and systemic characteristics with impant failure were evaluated by using Cox proportional hazards regression models and summarized with hazard ratios and 95% confidence intervals.
Results: The study consisted of 6,358 patients with a median age of 53 years at placement of the first implant. A total of 713 patients experienced implant failure at a median of 0.6 years. Among the 5,645 patients who did not experience implant failure, the median duration of follow-up was 5.8 years. 21 systemic conditions or systemic diseases were identified for assessment and 50% of the population had neither and served as a robust control. However, only 15 comprised more than 50 patients and 5 comprised more than 500 patients. The results had been adjusted for age, sex, and era of implant due to the influence of such factors on failure. The study main result is that no systemic disease or condition shown to increase the risk for implant failure in the population and settings studied.
Discussion: The study had adjustments for the risk models that would include variables affecting implant survival. This adjustment prevents assignment of risk due to confounding and may explain differences in risk estimates compared with those in other publications. However, after adjustment only the presence of coronary artery disease at the first implant was significantly associated with implant failure, and the association favored implant survival.
Conclusion: The study provides practice-based estimates for implant-failure risk that are related to the demographic, systemic disease or condition profiles of patients. The main finding was that no systemic disease or condition increased the risk of implant failure.
Topic: Medical Overview
Title: Systemic risk factors for peri-implant bone loss: a systematic review and meta-analysis.
Source: Int J Oral Maxillofac Surgery. 2014; 43:323-334.
DOI: 10.1016/j.ijom.2013.11.012
Type: Systematic Review
Keywords: bone loss; dental implants; meta-analysis; risk factors; smoking; systemic diseases
Purpose:
- The aim of this study was to determine the influence of patient-related systemic risk factors (systemic disease, genetic traits, chronic drug or alcohol consumption, and smoking status) on peri-implant bone loss at least 1 year after implant installation and prosthetic loading.
Methods:
- An electronic search was performed of MEDLINE, EMBASE, and The Cochrane Central Register of Controlled Trials up to January 2012. One thousand seven hundred and sixty-three studies were identified. After applying a three-stage screening process, 17 articles were included in the qualitative analysis, but only 13 in the quantitative analysis, since smoking was a common exposure.
Results:
- A total of 1883 patients and 5730 implants were analyzed.
- Cigarette and tobacco smoking were the most prevalent exposures (identified as single factors in 11 studies). The others were osteoporosis, IL-1 gene polymorphisms, diabetes, endocrine diseases, cardiac diseases, and arthritis, and Sjogren’s syndrome.
- Radiographic bone loss was evaluated by means of intraoral apical X- rays in 11 studies, panoramic X- rays in four studies, and both methods were used in two studies.
- Only a few studies reported soft tissue outcomes (bleeding on probing, plaque index, gingival recession, and width of keratinized tissues
- No study reported data for peri-implant gingival recession or width of keratinized tissues.
- The meta-analysis of these 13 studies (478 smokers and 1207 non-smokers) revealed a high level of heterogeneity and that smoking increases the annual rate of bone loss by 0.164 mm/year.
Conclusion:
- Exposure to smoking had a harmful effect on peri-implant bone loss. However, the level of evidence for oral implant therapy in patients with systemic conditions is very low. Future studies should be improved in order to provide more robust data for clinical application.
Title:Patient selection for endossous dental implants; Oral and systemic considerations.
Author:Sugerman, P., Barber, M
Source:J Oral Maxillofac Implants. 2002 Mar-Apr; 17(2):191-201
Type:Discussion
Rating: Good
Keywords:patient selection, endossous dental implant, oral, systemic consideration
Purpose:The aims of this article were to define “reasonable health” for dental implant treatment and to provide a systematic approach to the selection of dental implant patients.
Discussion:
TITANIUM TOXICOLOGY The survival or success of endosseous dental implants may be influenced by a number of local and systemic conditions. Some of these conditions affect the process of osseointegration directly. The following are noted in particular.
- PHYSICAL STATUS
- The American Society for Anesthesiology (ASA) has defined a 6-point scale of physical status
- AGE
- Younger patients may show greater crestal bone resorption around dental implants.It is therefore recommended that implant placement be delayed until growth and development have ceased or are minimal
- However, implant failure does not correlate with age or sex. Increasing age has no effect on osseointegration or the rate of crestal bone resorption around dental implants.
- PATIENT EXPECTATION
- Although dental implants can enhance esthetics, phonetics, and bite force, it is important to identify unrealistic expectationsthat patients may have about implants and implant- retained prostheses.
- HYPOHIDROTIC ECTODERMAL DYSPLASIA is characterized by hypodontia, hypotrichosis, and hypohidrosis. Dental implants have been used successfully in patients with severe hypodontia associated with ectodermal dysplasia.In a recent prospective study, implant placement and prosthetic rehabilitation in young children with ectodermal dysplasia did not restrict transverse or sagittal growth. However, vertical alveolar growth resulted in the occasional submergence of endosseous implants, necessitating revision and the placement of longer abutments.
- SMOKING:Many studies have shown that smoking interferes with osseointegrationand accelerates bone resorption around dental implants
- OSTEOPOROSIS:osteoporosis appears not to influence implant survival.Moreover,endosseous dental implants may actually stimulate mandibular bone formation in a load-dependent manner.
- DIABETES MELLITUS: endosseous dental implants are usually successful in patients with diabetes, although uncontrolled diabetes contraindicates dental implant placement. Consideration should be given to antibiotic prophylaxis for surgical procedures in diabetic patients.
- SCLERODERMA:little is known about dental implants in patients with scleroderma.Endosseous dental implants may improve prosthesis function and comfort in scleroderma patients, although access for implant surgery and for oral hygiene may be compromised.
- SJÖGREN SYNDROME: Implant-supported prostheses were shown to considerably increase prosthetic comfort and function in patients with Sjögren syndrome,preferable to soft tissue-supported prostheses.
- MULTIPLE MYELOMA: Implant success has been reported in a patient with multiple myeloma.Unmanaged malignant disease in general must be considered a contraindication for the placement of endosseous dental implants.
- PARKINSON’S DISEASE: Implant- supported prostheses should be considered in patients with Parkinson’s diseaseand other diseases affecting orofacial motor function.
- BONE MARROW TRANSPLANTATION: Implant placement should be delayeduntil cytotoxic chemotherapy has ended and the mar- row graft has taken. Bone marrow transplant patients may develop oral graft-versus-host disease that is clinically similar to oral lichen planus
- HIV: endosseous dental implants have been placed successfully in HIV-positive patients
- SYSTEMIC DRUGS: Consultation with the patient’s physicianprior to dental implant placement is desirable for patients on anticoagulants or long-term systemic corticosteroids.
- CHRONICALLY INFECTED IMPLANT SITES: Periodontitis and periapical lesions should be diagnosed and treated prior to dental implant placement.
- ORAL LICHEN PLANUS Endosseous dental implants may be used in patients with nonerosive forms of OLP, although patients should be warned of possible lesion exacerbation related to surgery and possible implant failure if gingival lesions become erosive
- HEAD AND NECK RADIOTHERAPY: Implant placement following head and neck radiotherapy is associated with a significant risk of osteoradionecrosis, especially with irradiation above 50 Gy. Recommended a 6- to 12-month recovery period after irradiation prior to dental implant placement
Presurgical hyperbaric oxygen may reduce the dental implant failure rate in irradiated jawbone from 60% to 5%
- TARDIVE DYSKINESIAS Tardive dyskinesia may complicate dental implant therapy.Alternatives to endosseous dental implants should be considered for patients with neurologic disorders including orofacial dyskinesia, trigeminal neuralgia, or orofacial dysesthesia.
Smoking
Topic:Risk factors for implants
Title:How do smoking, diabetes and periodontits affect outcomes of implant treatment?
Source:Int J Oral Maxillofac Implants. 2007; 22 (suppl)173-202
Type:Review
Rating: Good
Keywords:dental implants, dental implant survival, diabetes, periodontitis, smoking, tobacco
Purpose: To evaluate the available literature to assess whether smoking, diabetes, and periodontitis have an adverse effect on the outcomes of implants placed in patients with these conditions.
Method: The dental literature was searched using the MEDLINE, Cochrane Collaboration, and EMBASE databases. Using specific inclusion and exclusion criteria, 2 reviewers evaluated titles, abstracts, and full articles to identify articles relevant to this review. All searches were conducted for articles published through May 2005. Data from included articles for each of the risk factor groups, smoking, diabetes, and periodontitis, were abstracted and analyzed.
Results: A detailed search of the literature and evaluation of relevant articles identified 35 articles for inclusion in this systematic review. Nineteen articles were identified for smoking, 4 articles were identified for diabetes, and 13 articles were identified for periodontitis. One article met the criteria for both smoking and periodontitis. Implant survival and success rates were reported for smokers versus nonsmokers; diabetic patients versus nondiabetic patients; and patients with a history of treated periodontitis versus patients with no history of periodontitis. The findings revealed statistically significant differences in survival and success rates for smokers (better for nonsmokers), with greater differences observed when the data were analyzed according to bone quality (less for loose trabecular bone). No difference in implant survival rate was found between patients with and without diabetes. Likewise, no difference in implant survival rates was found between patients with a history of treated periodontitis compared to patients with no history of periodontitis.
Conclusion: The results of this systematic review of the literature demonstrated that smoking has an adverse effect on implant survival and success. The effect of smoking on implant survival appeared to be more pronounced in areas of loose trabecular bone. Type 2 diabetes may have an adverse effect on implant survival rates, but the limited number of studies included in this review do not permit a definitive conclusion. A history of treated periodontitis does not appear to adversely affect implant survival rates but it may have a negative influence on implant success rates, particularly over longer periods.
Topic:smoking and implant
Authors:Strietzel FP, Reichart PA, et al.
Title: Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis.
Source:J Clin Periodontol. 2007 Jun;34(6):523-44. Review.
Type: Retrospective Study
Rating: Good
Keywords:dental implants; meta-analysis;odds ratio; smoking; success rate; survival rate
P: To investigate if smoking interferes with the prognosis of implants with and without accompanying augmentation procedures compared with non-smokers.
A systematic electronic and handsearch (1989 and 2005; English and German language; search terms “dental or oral implants and smoking”; “dental or oral implants and tobacco”) was performed to identify publications providing numbers of failed implants, related to the numbers of smokers and non-smokers for meta-analysis. Publications providing statistically examined data of implant failures or biologic complications among smokers compared with non-smokers were included for systematic review.
R: Of 139 publications identified, 29 were considered for meta-analysis and 35 for systematic review. Meta-analysis revealed a significantly enhanced risk for implant failure among smokers [implant-related odds ratio (OR) 2.25, confidence interval (CI(95%)) 1.96-2.59; patient-related OR 2.64; CI(95%) 1.70-4.09] compared with non-smokers, and for smokers receiving implants with accompanying augmentation procedures (OR 3.61; CI(95%) 2.26-5.77, implant related). The systematic review indicated significantly enhanced risks of biologic complications among smokers. Five studies revealed no significant impact of smoking on prognosis of implants with particle-blasted, acid-etched or anodic oxidized surfaces.
C: Smoking is a significant risk factor for dental implant therapy and augmentation procedures accompanying implantations.
Topic: Patient Factors ( smoking)
Author: V. Moraschini , E. dS. PortoBarboza
Title: Success of dental implants in smokers and non-smokers: a systematic review and meta- analysis Source: Int. J. Oral Maxillofac. Surg. 2016; 45: 205–215
DOI: http://dx.doi.org/10.1016/j.ijom.2015.08.996
Type: Systematic Review
Keywords: dental implants; smoking; tobacco; implant survival; marginal bone loss; meta- analysis.
Purpose: Thepurposeofthisreviewwastotestthenullhypothesisofnodifferencein marginal bone loss and implant failure rates between smokers and non-smokers with respect to the follow-up period.
Methods An extensive electronic search was performed in PubMed, Web of Science, and the Cochrane Central Register of Controlled Trials to identify relevant articles published up to February 2015. The eligibility criteria included randomized and non-randomized clinical studies. After an exhaustive selection process, 15 articles were included. The meta-analysis was expressed in terms of the odds ratio (OR) or standardized mean difference (SMD) with a confidence interval (CI) of 95%.
Results: There was a statistically significant difference in marginal bone loss favouring the non-smoking group (SMD 0.49, 95% CI 0.07– 0.90; P = 0.02). Independent analysis revealed an increase in marginal bone loss in the maxilla of smokers, compared to the mandible (SMD 0.40, 95% CI 0.24–0.55; P < 0.00001). A statistically significant difference in implant failure in favour of the non-smoking group was also observed (OR 1.96, 95% CI 1.68–2.30; P < 0.00001). However, the subgroup analysis for follow-up time revealed no significant increase in implant failure proportional to the increase in follow-up time (P = 0.26).
Discussion: This review attempted to identify studies comparing the marginal bone loss and rate of implant failure between smokers and non-smokers.
Tobacco smoking is an accepted potenttial risk factor for oral health. Several clinical studies have shown that the sur- vival of implants can be affected by to- bacco usage. However, the quantity and frequency of cigarettes consumed (or packs per year) can be a key factor in determining the predictability of the implants.
Conclusion- a statistically significant difference in marginal bone loss was found between the smoking group and the non-smoking group, in favour of the non-smoking group (SMD 0.49, 95% CI 0.07–0.90; P = 0.02).
Topic: Smoking and dental implants
Title: Smoking and dental implants: A systematic review and meta-analysis
Source: Elsevier Journal of Dentistry
DOI: https://doi.org/10.1016/j.jdent.2015.03.003
Type: Systematic review and Meta analysis
Keywords: Dental implants, smoking, systematic review, meta-analysis, implant failure rate, postoperative infection, marginal bone loss.
Purpose:To test the null hypothesis of no difference in the implant failure rates, postoperative infection, and MBL for smokers or non-smokers, against the alternative hypothesis of a difference.
Methods:For this review, patients smoking minimum of one cigarette per day were classified as smokers. Definitions:Implant failure = complete loss of the implant. Exclusion: Case reports, technical reports, biomechanical studies, finite element analysis, animal studies, in vitro and review papers.
Results: Search resulted in 1432, after duplicates and paper that met exclusion a total of 107 publications were included in the review. 4 Randomized Clinical trials, 16 prospective studies, 71 retrospective analyses.
From 104 studies comparing implant failure rates: A total of 19,836 implants were placed in smokers, with 1,259 failures (6.35%), 60,464 implants were placed in non-smokers, with 1923 failures (3.18%)., 44 studies informed there was a statistically significant difference between failure rates amd 17 did not find statistically significant difference.
- The insertion of dental implants in smokers statistically affected the implant failure rates; implying that it is 2.23 (123%) times more likely to fail.
- Statistically affected incidence of postoperative infections (RR=2.01) and marginal bone loss.
After a sensitivity analysis was performed:
- When placed in the maxilla statistically affects implant failure rates
- When placed in the mandible, no statistically difference.
- Significant difference when using turned implants with sandblasted and acid etch surfaces.
- The study suggests that insertion of implants in smokers affects failure rates, risk of postoperative infection and marginal bone loss, mainly because the effect of smoking in osteogenesis and angiogenesis.
- Nicotine inhibits gene expression of several enzymes that regulate osteoblast proliferation, differentiation and, apoptosis; which affects bone formation and remodeling.
- Nicotine has local and systemic effects on blood vessels, producing vasoconstriction, resulting in decreased blood perfusion and causing ischemia.
- There is evidence to suggest that smoking may have dose-related effect on osseointegration, however, few studies reported quantity of cigarettes and reported the number of years smoking.
- A 60 month follow-up success rate for non smokers was 82.7% and for smokers was 65.3%.
Conclusion: Results should be interpreted with caution due to the presence of uncontrolled factors. Present study suggest that smoking affect implant failure rates, post-operative infection.
Topic:smoking and implant
Title:Implant installation in the smoking patient.
Source:Periodontol 2000. 2003;33:185-93.
Type:Review.
Rating: good
Keywords:implant, failure, smoking,
Purpose:to review the association between smoking and implant failure; potential mechanisms, and benefits of smoking cessation.
Discussion:
- Effects of smoking on general health:smoking has been shown to affect health in many ways such as; cancers especially lung cancer, chronic lung disease, myocardial infarctions, strokes and ischemic heart disease. Research show that 50% of smokers die from a smoking related disease, and life expectancy of smokers is reduced by 7.5 years. Smoking also has been shown to have an adverse effect on bone density.
- Effects of smoking on wound healing: smoking is a complicating factor in post-surgical wound healing. Smokers show less reduction in PD after SRP, poorer healing after mucogingival surgeries, less favorable healing following OFD, greater loss of bone height, reduction in post-ext socket fill and more painful ext socket. Smoking compromises healing of duodenal ulcers. Also, in a study about healing after orthopedic surgery, it was shown than there are more delayed union or non-unions in smokers.
- Influence of smoking on the actions of polymorphonuclear leukocyte, macrophages, circulation and blood flow:Several studies have shown that smoking causes reduced phagocytosis, delayed margination and diapedesis as well as compromised aggregation and adhesion of leukocytes to the endothelium in venules and arteries. Peripheral endothelial dysfunction, vessel wall injury and capillary loss is common in smokers, also reactive hyperemia and sequestration of blood cells in the microcirculation. Coronary flow reserve is also decreases after smoking high-nicotine cigarettes.
- Smoking and implant failure:
- Smoking and particularly heavy smoking increases the failure rates for machined titanium implants, likely due to a compromise of the blood supply in bone during early healing
- This increased failure rate clusters largely in the maxilla, with much smaller differences between smokers and non-smokers for implant in the mandible.
- Smoking is associated with a particularly high failure rate for implants placed into grafted maxillary sinuses.Some operators may consider this to be too great a risk to take, if the patient is unable or unwilling to stop smoking.
- What happens if the potential implant patient stops smoking:Smoking cessation has been demonstrated to improve success rates in machined implant patients. In fact, implant placement may well be an effective motivator in assisting a smoker with cessation.
- Bone density, smoking and implant success: There appears to be a relationship between heavy smoking and reduced bone density. This is seen in various areas of medicine, as well as in implant surgery and might explain high failure rates in Type 4 bone
- Do different materials and surfaces make a difference:There is early evidence that rough surface implants, prepared with a double acid etched technique, have a high success rate in smokers. With success rates around 10% better overall (98.7% vs. 88.7%) and 15% better in the maxilla (97.3% vs. 82.1%) than our original results with machined Branemark implants in smokers, these are at present considered to be the implant of choice in smokers who cannot or will not stop smoking for implant placement.
Topic: Implant Risk Factor-Smoking
Authors: Naseri R, Yaghini J, Feizi A
Title: Levels of smoking and dental implants failure: A systematic review and meta-analysis
Source: J Clin Periodontol. 2020 Apr;47(4):518-528
DOI: 10.1111/jcpe.13257
Type: Systematic Review/Meta
Keywords: implant, failure, smoking, meta-analysis
Purpose: To investigate if there was a significantly enhanced risk of dental implant failure due to the increased number of cigarettes smoked per day.
Material and methods: In accordance with PRISMA. Electronic search (PubMed, EMBASE, Web of Science, Scopus upto January 2019)
Results: 23 studies in both qualitative and quantitative study
- Meta-analysis based on implant-related data (higher implant failure rate)
- Group I (none, <10, or >10):
- SS, (>10) > (<10) > non-smoker
- Group II (none, <15, or >15):
- No SS b/t <15 and non-smoker
- SS, (>15) > non-smoker
- No SS b/t <15 and >15
- Group III (None, <20, or >20):
- SS, (<20) > non-smoker
- SS, (>20) > non-smoker
- No SS, <20 and >20
- Group IV (None, 1-10, 10-20 or >20):
- SS, (<10) > non-smoker
- SS, 10-20 > non-smoker
- SS, (>20) > non-smoker
- No SS, (<10) and (10-20)
- SS, (>20) > (10-20)
- Meta-analysis based on patient-related data (at least one implant in a patient failed)
- Group I (None, <10 or >10):
- No SS, (<10) and non-smoker
- SS, (>10) > non-smoker
- No SS, (<10) and (>10)
- Group II (None, <15 or >15):
- No SS, (<15) and non-smoker
- SS, (>15) > non-smoker
- No SS, (<15) and (>15)
- Group III (None, <20 or >20):
- SS, ((<20) or (>20)) > non-smoker
- No SS, (<20) and (>20)
- Group I (None, <10 or >10):
- Group I (none, <10, or >10):
Discussion:
- Based on the findings
- Study demonstrated an increase in the Relative Risks of implant failure in all smoker subgroups than in non-smokers. The findings showed the more cigarettes smoked daily, the more probable was the dental implant failure.
- Smoking <10 cigarettes/day can be “recommended” tolerated with caution as a safe level against dental implant failure.
- Smoking more than one pack/day can be considered a risk factor for implant failure.
- The domain of 10–20 cigarettes smoked per day is an uncertain range for implant failure. It seems that implant failure operates along a continuum with no apparent threshold of smoking level. It is recommended that cigarette consumption data be analyzed as a continuous rather than as a categorical variable in the future studies
- Patient-related analysis confirms implant-related analysis.
- When implant failure is calculated with the patient as the statistical unit, the statistical methodology can overestimate the outcome
- More negative outcome for patients with multiple implants because when one implant is failed in a patient with multiple implants, the patient’s treatment outcome is considered a failure
- Half of the papers included in the meta-analysis had short-term follow-up period, lower than 2 years.
- When implant failure is calculated with the patient as the statistical unit, the statistical methodology can overestimate the outcome
Topic: Implants and tobacco use
Authors: Javed F., Rahman I., Romanso GE.
Title: Tobacco-product usage as a risk factor for dental implants
Source: 10.1111/prd.12282
DOI: 10.1111/prd.12282
Type: Review article
Keywords: alveolar bone loss, dental implant, inflammation, osseointegration, smoking
Review:
Tobacco use: A risk factor for peri-implant diseases
- Along with poor OH, hx perio disease, immunocompromised status, and occlusal loading, habitual use of tobacco products is a significant risk factor for peri-implant diseases.
- Several investigations have demonstrated that:
- Smoking is a SS predictor of implant failure.
- Smokers experience SS higher rates of implant failure, post-op infection, and crestal bone loss.
- Type IV bone is more commonly found in smokers.
Nicotine: Definition and its deleterious effects on oral and systemic health
- 90% of nicotine is metabolized by the liver, lungs, and kidneys.
- Conc of nicotine in GCF 300x higher than serum.
- Nicotine has vasoconstrictive effects, which may result in reduced BOP in smokers.
- High conc of nicotine and cotinine inhibit proliferation of gingival fibroblasts and their adhesion to root surfaces, compromising CAL, while enhancing proliferation of osteoclasts, increasing alveolar bone loss.
- Increased glycation in periodontal tissues may compromise outcomes of periodontal surgical interventions.
- Nicotine has also been associated with several systemic diseases (acute cardiac ischemia, atherosclerosis, coronary artery disease, HTN, thrombosis).
Effect of nicotine on osseointegration: Lessons from animal studies
A limited number of animal studies demonstrate:
- A SS decrease in bone-to-implant contact at 4 weeks in rats exposed to nicotine.
- Deceased bone volume around implants in rats receiving subcutaneous nicotine injections.
- Several studies demonstrate no differences in bone-to-implant contact.
- However, these results should be interpreted carefully, as nicotine was delivered subcutaneously, and nicotine absorption has been shown to faster via inhalation.
Success and survival of implants and tobacco product usage
- Cigarette smoking
- A classical risk factor for both peri-implant diseases and implant failure.
- Peri-implant marginal bone loss SS higher in smokers due to upregulation of inflammatory cytokines.
- Controversial results have also been reported, demonstrating no significant differences in smokers.
- One study showed 97% vs 99% implant survival for immediately loaded platform-shifted implants placed in smokers and non-smokers, respectively.
- A classical risk factor for both peri-implant diseases and implant failure.
- Waterpipe smoking (hookah)
- HTN, tachycardia, oxidative stress, lung cancer, oral cancer, periodontal disease, and alveolar bone loss have been associated with waterpipe smoking.
- Individuals are exposed to the same toxic chemicals as cigarette smoking
- No studies have directly studied waterpipe smoking and implant related outcomes, however waterpipe smoking is likely a significant risk factor for peri-implant diseases.
- Pipe and cigar smoking
- Similar to waterpipe smoking, pipe and cigar smoking exposes individuals to the same toxic chemicals as cigarettes.
- Studies have demonstrated pipe/cigar smoking to be less detrimental than cigarette smoking; however, poor systemic and oral health and an association with periodontitis has been shown.
- Similar to waterpipe smoking, pipe and cigar smoking exposes individuals to the same toxic chemicals as cigarettes.
- Electronic cigarette vaping
- No clinical studies exist examining periodontal or peri-implant outcomes.
- Experimental evidence indicates e-cigarettes may negatively influence outcomes of dental implant therapy similar to conventional smoking.
- Smokeless tobacco use
- An abundance of evidence shows a direct association between smokeless tobacco products and oral malignancies.
- All types of smokeless tobacco have been shown to be equally hazardous to periodontal health.
- It is hypothesized that peri-implant PDs and marginal bone levels are worse in smokeless tobacco users than nonsmokers, and implant placed proximal to the placement of the smokeless tobacco product exhibit worse clinical parameters.
Tobacco products and dampening of innate immune responses in survival/failure of dental implants
- Tobacco use has been shown to dampening of innate immunity by activation of the nuclear factor kappa B pathway and toll-like receptors, which triggers various inflammatory mediators and oxidative stress.
- This culminates in damage to the peri-implant tissues and may lead to per-implant diseases and implant loss if untreated.
- Pt education on the effects of all tobacco products is the responsibility of healthcare providers.
Conclusion:
While evidence on the success and survival of dental implant in tobacco users is scarce in volume, the demonstrated deleterious effects of tobacco use cannot be ignored and must be highlighted in patient care. Routine pt education is highly recommended.
Diabetes
Topic: implants and diabetics and CVD
Author: Nobre, MA, Malo, P, Goncalves, Y, Sabas, A, Salvado, F.
Title: Outcome of dental implants in diabetic patients with and without cardiovascular disease: a 5-year post-loading retrospective study.
Source: Eur J Oral Implantol. 2016; 9(1): 87-95
DOI:
Type: Retrospective clinical study
Keywords: dental implant, diabetes, cardiovascular disease, risk factor, marginal bone loss
Purpose: To look at the outcomes of immediately loaded implants in diabetic patients with or without coexisting cardiovascular disease at 5 years.
Methods: Retrospective study of private practice patients in Portugal. 70 patients with diabetes who were treated between 1999-2007 were included. Patients were divided into 2 groups:
- Diabetes and coexisting CVD
- Diabetes without coexisting CVD
Clinical and radiographic examinations were done to plan the implants. Standard surgical procedures were followed to place NobelSpeedy implants. Sites were underprepared to achieve insertion torque of 30Ncm. For single teeth, final abutments were placed the day of surgery and temporary screw retained crowns were delivered into immediate function. Full arch patients received full-arch acrylic resin prosthesis at the day of surgery. Typically, final restorations were delivered after 6 months. Follow-ups were performed at 10days, 2, 4, and 6months after surgery and every 6 months thereafter. Radiographs were taken in order to measure MBL at baseline, first year and fifth year.
Results: 70 diabetic patients (38 with CVD and 32 without CVD) were included in the study. The groups included some smokers, bruxers and those with history of periodontitis.
- Diabetics with CVD: received 183 dental implants
- Diabetics without CVD: received 169 dental implants
Cumulative Prosthesis and implant survival rates:
- Diabetics with CVD:
- Prosthesis survival: 100%
- Implant survival: 8%
- Diabetics without CVD
- Prosthesis survival: 97.4%
- Implant Survival: 86.7%
Marginal Bone Loss and Complications: Average MBL at 1 and 5 years was 0.88mm and 1.56mm respectively. NSSD was seen between groups.
1) Diabetics with CVD:
- MBL 1 year: 0.95mm
- MBL 5 years: 1.52mm 2) Diabetics without CVD:
- MBL 1 year: 0.78mm
- MBL 5 years: 1.54mm
Complications occurred in 38 patients. 7 patients experienced biologic complications being primarily periimplant pathology and were treated either non-surgically or surgically. Mechanical complications occurred in 33 patients and included temporary prosthesis fracture, definitive prosthesis fracture, and prosthesis loosening. No significant differences were seen with complications between groups.
Discussion: The authors concluded that NSSD were found between diabetics with and without CVD in regard to dental implant therapy with immediate load. They concluded there is a favorable risk-benefit ratio for treatment at 5 years.
Topic: diabetes
Authors: Naujokat H, Kunzendorf B, Wiltfang J.
Title: Dental Implants and diabetes mellitus-a systematic review.
Source: Int J Implant Dent. 2016 Dec;2(1):5
DOI: 10.1186/s40729-016-0038-2
Type: systematic review
Keywords: Dental implants; Diabetes mellitus; Glycemic control; Implant survival; Peri-implantitis; Risk factor; Systemic disease
Purpose: To determine if diabetic patients with dental implants have a higher complication rate in comparison to healthy controls.
Methods: an online search in the literature was conducted. 22 studies out of a total of 327 were included in this review. Because of too few studies, heterogenic study design, and incompletely reported data like type of diabetes therapy, quality of glycemic control, and duration of disease, the quantitative data synthesis could not be performed in the way necessary for meta-analysis. In most of the studies, patients were divided into: well-controlled (HbA1c 6.1– 8 %), moderately controlled (HbA1c 8.1– 10 %), and poorly controlled (HbA1c ≥ 10 %). The healthy control had HbA1c ≤ 6 %.
Results:
- Dental implants are safe and predictable procedures for dental rehabilitation in diabetics.
- The survival rate of implants in diabetics does not differ from the survival rate in healthy patients within the first 6 years, but in the long-term observation up to 20 years, a reduced implant survival can be found in diabetic patients.
- Patients with poorly controlled diabetes seem to have delayed osseointegration following implantation. After 1 year, there is no difference between diabetic and healthy individuals, not even to the poorly controlled HbA1c. Therefore, authors recommend avoiding immediate loading of the implants.
- In the first years after implant insertion, there seems to be no elevated risk of peri-implantitis; but in the long-term observation, peri-implant inflammation seems to be increased in diabetic patients. Therefore, a risk-adapted dental recall is helpful to detect early signs of gingivitis, which can easily be treated by dental/implant cleanings to avoid serious peri-implant infection.
- Authors found some hints that good glycemic control improves osseointegration and implant survival. Therefore, and to avoid other long-term side effects, the practitioner should ask for the HbA1c and if necessary improvement of antidiabetic therapy should be aimed.
- In the literature, there was no evidence that bone augmentation procedures like guided bone regeneration and sinus lifts have a higher complication and failure rate in patients with well- to fairly well-controlled diabetes. To improve implant survival and reduce postoperative complications, supportive therapy consisting of prophylactic antibiotics and chlorhexidine mouth rinse is recommended.
Conclusion: patients with poorly controlled diabetes suffer from impaired osseointegration, elevated risk of peri-implantitis, and higher level of implant failure. The influence of duration of the disease is not fully clear. The supportive administration of antibiotics and chlorhexidine seems to improve implant success. When diabetes is under well control, implant procedures are safe and predictable with a complication rate similar to that of healthy patients.
Topic: Diabetes
Authors: Monje A, Catena A, Borngakke WS
Title: Association between diabetes mellitus/hyperglycemia and peri-implant disease: systematic review and meta-analysis.
Source: J Clin Periodontol. 2017 Jun;44(6):636-648.
Type: Review
Keywords: dental implants; diabetes complications; epidemiology; gestational diabetes
Purpose: to identify and assess the existing scientific evidence from epidemiologic, non-experimental, observational studies of associations between hyperglycemia/ diabetes mellitus and peri-implant disease through systematic review.
Methods: electronic and manual literature searches were conducted independently by 2 authors. Inclusion criteria included: humans whose peri-implantitis or peri-implant mucositis was clinically diagnosed. Cases were defined by hyperglycemia and a normoglycemic comparison group. Results needed to include at least one parameter related to hyperglycemia and report presence of peri-implant mucositis or peri-implantitis. Other inclusion criteria included overall enrollment of atleast 10 subjects, duration of atleast 6 months, and rough surface screw-shaped implants.
Results: 12 studies out of 401 titles were included. 5 were prospective cohort studies, 1 retrospective cohort study, and 6 cross-sectional studies. These studies included 1,955 participants; 12 with pre-diabetes, 468 with diabetes, and 1,487 with no diabetes. 2, 892 implants were assessed. 3 of the prospective studies were eliminated due to heterogenicity compared to the rest of the reported data. 7 out of the 9 remaining studies could be synthesized by meta-analysis to assess the association between hyperglycemia/ diabetes and peri-implantitis.
Peri-implant mucositis did not have OR or RR between hyperglycemia vs. normoglycemia. However, Periimplantitis had both OR and RR statistically significantly higher in hyperglycemia than in normoglycemia.
| The risk of peri-implantitis in hyperglycemia is between 1.21 and 2.46 fold statistically significantly higher | |
| than in normoglycemia. | |
No study reported prevalence of peri-implant diseases in hyperglycemia vs otherwise healthy subjects without other confounder factors (smoking, history of periodontitis, or poor plaque control). 3 studies among non-smokers exclusively report consistent results as they all find subjects with hyperglycemia to have about 3x greater risk of peri-implantitis compared to normoglycemia.
Conclusion: Similar mechanisms are activated in peri-implant tissues as around natural dentition in periodontitis. Limitations of conducting this review is the heterogenicity of peri-implantitis definition. The patient should be made aware of risk involved in implant therapy with hyperglycemia.
Osteoporosis and/or Bisphosphonates
Topic:osteoporosis
Authors:Holahan, C et al
Title:Effect of osteoporotic status on the survival of titanium dental implants.
Source: Int J Oral Maxillofac Implants. 2008:Sep-Oct; 23(5)905-10
Type:
Keywords: dental implants, implant survival, osteoporosis
Purpose:Primary Objective is to perform a retrospective chart review to determine the effect of osteoporotic status on survival of dental implants in postmenopausal women. Secondary Objectives included assessing the effects of smoking status, age, and arch location on implant survival as a function of osteoporotic status.
Method: a retrospective chart review was completed on all women who were 50 years of age or older at the time of dental implant placement at the Mayo Clinic between Oct 1, 1983 and Dec 31, 2004. The medical and dental charts were evaluated to collect the following:
- BMD T-score within 3 years of implant placement
- Osteoporotic diagnosis based on BMD T-score
- Arch location of the implants
- Smoking status at time of implant placement
- Any implant failures (implant removal due to any reason other than infection or manufacturing defects)
The review resulted in 192 patients (646 implants). Implant survival was estimated using the Kaplan-Meier method. Follow up duration was calculated from date of implant placement to date of failure or last follow up.
Results:
- The Kaplan-Meier t- and 10-year survival rates for the 64 implants in 192 patients were 93.8% and 92.5% respectively. The mean follow up was 5.4 years (range 11 days to 20.4 years). Mean age of women studied was 63.4 years (range 50.3 to 84.9 years)
- Osteoporotic diagnosis of patients based on BMD T-score was: 49% diagnosed as non-OP, 29.7% had osteopenia and 21.4% had osteoporosis. 37 implant failures were found: 10 implant failures in the osteoporosis group, 10 implant failures in the osteopenia group and the other 17 failures occurred in patients with non-OP diagnosis.
- No significant association between arch location and implant failure was identified.
- 12.5% of patients were smoking at the time of implant placement. Smoking had a significant effect on implant failure. Implants in smokers were 2.6 times more likely to fail (5- and 10- year implant survival rate for smokers was 87.3%). Non-smokers had 94.6% and 93.1% survival rates.
Conclusion:
- Dental implant survival rates in this group of patients were encouraging with a 10-year survival rate of 92.5%.
- Implants placed in smokers were 2.6 times more likely to fail than those placed in nonsmokers. The difference between those were most evident in the first year after implant placement.
- A diagnosis of osteoporosis or osteopenia is not a contraindication to dental implant therapy.
Topic: Osteoporosis/osteopenia
Author: Temmerman A, Rasmusson L, Kubler A, Thor A, Merheb J, Quirynen M
Title: A prospective, controlled, multicenter study to evaluate the clinical outcome of implant treatment in women with osteoporosis/osteopenia: 5-year results
Source: J Dent Research 2019, Vol. 98(1) 84–90
DOI: 10.1177/0022034518798804
Type: clinical
Keywords: dental implants, marginal bone loss, postmenopausal, long-term outcome, survival rates, bone mineral density
Purpose: to provide long-term information on the clinical performance of oral implants in patients with diagnosed systemic primary osteoporosis/ osteopenia.
Background:
- Osteoporosis is defined as a skeletal disease, characterized by a low density of bone tissues
- Primary osteoporosis can be divided into 2 groups: post- menopausal osteoporosis and senile osteoporosis.
- Dual X-ray absorptiometry (DXA) is the gold standard in the diagnosis of osteoporosis/osteopenia. DXA scans assess the bone mineral density (BMD) and report a Tscore.
- T-score compares the BMD with the mean peak BMD for an individual of the same sex (healthy, 30-year-old individual).
- A T-score of 0 to −1.0 is considered nor- mal. A T-score of −2.5 or less will result in the diagnosis of osteoporosis, whereas T-scores of −1.0 to −2.5 are diagnosed as osteopenia. Methods:
- This study was performed at 4 centers: Leuven (Belgium), Gothenburg (Sweden), Würzburg (Germany), and Uppsala (Sweden)
- Patients were divided into 3 groups:
Group O (osteoporosis/osteopenia): patients with a T-score ≤ -2 o
Group C (healthy – control): patients with a T-score ≥ -1
- Inclusion: provision of informed consent, postmenopausal women aged ≥60 years, in need of 2- 8 implants in the maxilla, a history of edentulism in the area of oral implant therapy of ≥3 months, BMD suitable for group O or C (A: T-score ≥2 SD in g/cm3 and B: T-score ≥ -1 g/cm3)
- 2 – 8 implants (OsseoSpeed TX, Astra Tech Implant System; DentsplySirona) placed via 2-stage approach and Implants Stability Quotient (ISQ) were measured.
- PA radiographs taken immediately post-op and at 12 weeks when healing abutments were connected to the implants
- At 13 weeks, abutment level impression taken, and permanent restorations (bar-attached overdenture or screw-retained fixed partial denture [FDP]) was delivered 4 to 8 weeks after abutment surgery, and the implants were functionally loaded
- oral examination and implant follow- up were performed at 6 months after loading and then yearly up to 5 years. At every recall, intraoral PA radiographs were taken.
- Marginal bone levels (MBLs) were measured from a reference point (junction of the roughened and machined beveled surface) to the most coronal point of the bone-to-implant contact, both mesially and distally.
- The MBL at loading was regarded as baseline. Alterations were defined as the difference between MBL at base- line and each follow-up appointment
- Parameters (plaque scores, probing depth – PPD, bleeding on probing – BOP, clinical attachment levels CAL) of the peri-implant mucosa were recorded at every follow-up appointment and written down in the file of the patient
- Analysis was performed at implant level and patient level. Results:
- 148 implants placed in 48 patients (mean age: 67)
- 64 implants placed in group O (20 patients), 85 implants placed in group C (28 patients)
- 117 implants in 37 patients assessed at 5-year follow up
- The cumulative survival rate for all patients, after 5 y, on an implant level was 96.5% (group O:
91.5%; group C: 100.0%) and 95.7% (group O: 89.2%; group C: 100.0%) on a patient level.
- There was a significant difference in implant survival between groups O and C on an implant level (P = 0.004) but no significant difference on a patient level (P = 0.29).
- After 5 y of loading, 5 mechanical complications occurred (abutment screw fractures and connecting bar fractures), and 3 patients were treated for peri-implantitis.
- The overall MBL alterations on an implant level were −0.09 ± 0.78 mm (group O: −0.15 ± 0.50 mm; group C: −0.06 ± 0.89 mm).
- The overall MBL alterations on a patient level were −0.09 ± 0.54 mm (group O: −0.18 ± 0.43 mm; group C: −0.06 ± 0.58 mm)
- No significant difference in MBL alterations between loading and loading + 5 y between group O and group C, neither on an implant level (P = 0.31) nor on a patient level (P = 0.54)
- Smoking and type of restorations did not affect MBL alterations after 5 years of loading
- No statistically significant difference in plaque score, BOP, PPD, or CAL was found after 5 years of loading
Discussion:
- Oral implant therapy is a reliable treatment option in patients with osteoporosis, with survival rates and MBL alteration values comparable to the healthy control group. 50 vs 8.5% failure rate
Topic: osteonecrosis & bisphosphonates
Title: Osteonecrosis associated with dental implants in patients undergoing bisphosphonate treatment Source: Clin Oral Implants Res. 2014 May;25(5):632-640
DOI: 10.1111/clr.1208
Type: case study
Keywords: bisphosphonates, dental implants, jaw, osteonecrosis
Purpose: To verify clinical and pathological characteristics of BRONJ around dental implants, the present study analyzed clinical, radiographic and histopathological findings of these lesions.
Materials/Methods:
- 19 study subjects who were implant-treated patients, and developed BRONJ of the maxilla or mandible and were followed up for > 3 months o The demographic data, prior medical and dental history, duration, type, route of administration of BP were recorded.
- Surgical treatments related to implant placement and progress after the BRONJ treatment were analyzed.
- After confirming the diagnosis, the BRONJ patients were recommended to stop the BP treatment
- Surgery was performed when no change in BRONJ status was noted o Surgical curettage of necrotic bone was carried out for most of the patients. o implants were extracted when the necrotic bone surrounded more than half of the implant surface or the implant lost stability after curettage or sequestrectomy of the necrotic bone
- primary treatment outcomes were divided according to the condition of the lesion after primary treatment and were classified as follows:
- (i) Complete cover of mucosa over the lesion site;
- (ii) Mostly covered by mucosa but still had some part of asymptomatic exposed bone;
- (iii) Partial healing, exposed bone with symptoms such as pain, swelling, or pus discharge that requires further treatment
- Biopsy of all specimens taken
- primary treatment outcomes were divided according to the condition of the lesion after primary treatment and were classified as follows:
Results
- Oral BP users were most common (79%) compared with IV BP.
- Alendronate was the most commonly related drug.
- The lesion was located in mandible (n=9), maxilla (n=8) or both (n=2).
- BP initiation before surgery was documented in 16 people and after implant surgery in 3 people
- NSSD in period of drug administration, drug holiday, or location of the lesion in terms of sequestrum formation o extended bone resorption accompanying the bacterial colonies, as well as acute and chronic inflammatory cells were observed at the implant-surrounding bone tissue
Discussion/Conclusion:
- Only three patients developed osteonecrosis within 6 months after implant surgery, which suggests that the surgical process during the dental implant procedure is a contributing factor.
- Many patients (58%) developed BRONJ without any relation to surgical trauma from insertion or removal of the dental implant.
- could not find definitive relation between the BP duration and underlying disease and treatment outcomes.
- Most patients (68% of the cases) exhibited complete cover of mucosa after the first treatment using surgical curettage of necrotic bone or sequestrectomy.
Already osseointegrated dental implant also can show the osteonecrosis around the implant after BP administration.
Topic: Bisphosphonates
Author: Stavropoulos A, et al.
Title: The effect of antiresorptive drugs on implant therapy: systematic review and meta-analysis. Source: Clin Oral Implants Res. 2018 Oct;29 suppl 18:54-92.
DOI: 10.1111/clr.13282
Type: Meta-analysis
Keywords: antiresorptive drugs, bisphosphonates, dental implants, hormone replacement therapy, medication-related osteonecrosis of the jaw, systematic review
Purpose: To answer the question “In patients with systemic intake of ARDs, what is the outcome of implant therapy in terms of rates of implant loss, failure of grafting procedures, peri-implant marginal bone loss, MRONJ, and periodontitis compared to patients without systemic intake of ARDs?”
Methods: Electronic search including studies that were English or German, case series, cohort studies, case control studies, controlled and randomized clinical trials, retrospective design, greater than 10 patients with systemic intake of ARDs, clearly reported relevant clinical data.
Results:
- 36 articles were included in the study after all exclusions and grouped into studies on BP intake, studies on HRT intake, and studies on MRONJ associated with implants.
- Bisphosphonate Intake:
- No significant differences were observed regarding implant loss between cases and controls and success rates renaged from 85.7% to 100%.
- One study found an OR of 2.7 for implant loss with bisphosphonate intake o More implant losses were found in posterior maxilla, a short time from installation. o No SSD for marginal bone loss, one study reports an OR 3.3. for thread exposure o Several studies report no association with MRONJ and implants or grafting, but one study of 16,000 cases showed only 5 cases with complications.
- Hormone Replacement Therapy:
- Higher implant loss rate 9.1%-27.3% compared to conrols, a relative risk of 2.55 o 25% versus 15% of implant length bone loss comparing HRT with controls
- MRONJ Associated with Implants o Associated with bisphosphonate therapy in all studies except one o 84 in posterior mandible, 34 in maxilla
- 20 cases showed that implant installation or explantation as the trigger for MRONJ, and
41 cases showed the presence of the implant causing MRONJ o IV bisphosphonates were present in 61 cases, and oral in 44 cases.
- Meta Analysis:
- NSSD were observed in terms of implant loss between cases and controls in bisphosphonate studies.
- Hormone replacement therapy however, showed a marginally significant negative effect regarding implant survival on the patient level.
- MRONJ in patients on bisphosphonates for osteoporosis appeared >36 months after start of drug intake, while those on bisphosphonates for cancer had MRONJ <36 months after drug intake.
Discussion: Low-dose oral bisphosphonate intake for osteoporosis does not compromise implant therapy, they do not lose more implants or develop more complications compared to those not taking the drug. No relevant information exists on the effect of implnlat therapy on high-dose bisphosphates. Hormone replacement therapy has no negative effect on the implant level but may exert a marginally negative effect on implant survival and marginal bone levels. There is too little evidence to draw conclusions on grafting in conjunction with implants. There are valid reasons to consider as high-risk patients for MRONJ, those patients with high dose ARD intake for managing malignancies, patients on long term oral BP, and patients with comorbidities.
Topic: Implant survival and Medications
Authors: Ata-Ali J, Ata-Ali F, Peñarrocha-Oltra D, Galindo-Moreno P.
Title: What is the impact of bisphosphonate therapy upon dental implant survival? A systematic review and meta-analysis.
Source: Clin Oral Implants Res. 2016 Feb;27(2):e38-46.
DOI: 10.1111/clr.12526
Type: Systematic Review
Keywords: bisphosphonate-related osteonecrosis of the jaws, dental implant, failure, risk factor, success rate, survival rate
Purpose: To determine what impact bisphosphonate therapy has on dental implant survival.
Material and methods: Systematic review and meta-analysis. Electronic data search utilized, as well as manual search. 14 studies were included in the systematic review that met the inclusion criteria. Eight studies were included in the meta-analysis, six retrospective and two prospective studies. Statistical analysis then took place.
Results: 1288 participated in total, 386 patients receiving bisphosphonate therapy and 902 patient controls. 4562 DI were placed in total, 3472 DI were placed in patients without bisphosphonate therapy and 1090 DIs were placed in patients receiving bisphosphonate therapy. 26/1090 DIs failed in the test group. 76/3472 DIs failed in the control group. In the meta-analysis, the OR of 1.43 showed that enough evidence does not exist to show that BPs have negative effect on DI survival. The number needed to harm was 509 DIs.
Conclusions: This study determined that placing DIs in patients who have received bisphosphonate therapy does not cause a reduction in success rates of the DIs. Statistical significance was not reached, but the OR did suggest poorer results in the test group versus the control. Complications in patients receiving bisphosphonate therapy have been observed and need to be explained to the patient prior to surgery. Evaluation must be individualized, due to the serious but infrequent complication of bisphosphonate-related osteonecrosis of the jaw in patients with a history of BP therapy. Prospective studies with larger sample sizes and longer duration follow-up must be used in the future to confirm the results of the present study.
Radiation Therapy
Topic:Radiation
Authors: Colella, Cannavale, Pentenero, Gandolfo:
Title:Oral implants in radiated patients: A systematic review
Source:Int J Oral Maxillofac Implants 2007; 22(4):616-623
Type:Systematic review
Rating: Good
Keywords: Dental implants, oral cancer, radiation therapy
Purpose:To evaluate and compare the effects of pre- and post-implant radiation therapy. Incidence of implant failure was linked to multiple variables and assessed.
Methods:A thorough review of the relevant literature was performed. Studies were original studies based in humans from 1990- 2006. The man outcome considered was implant failure, defined as implant mobility, implant removal necessitated by progressive marginal bone loss or infection (biologic failure). Restorative status was not considered a determinate of success (sleeping implants were considered a positive outcome). Overall implant failure rate was compared for pre-implantation radiation therapy vs. post-implantation. Four variables were considered: implant location (maxilla vs. mandible), dose of radiation, delay from radiation to implant placement, and timing of implant failure.
Results:18 articles were considered eligible for inclusion in the review.Implant failure in post-implantation radiation therapy: 6 studies overall reported 124 implants with 4 failures (3.2%). Implant failure in pre-implantation radiation therapy: An overall failure rate of 5.4% was reported, which was not significantly different from post-implantation. 22/46 failures reported the cause of failure, with 9 due to lack of osseointegration, 12 due to marginal bone loss, and 1 due to biting trauma. Implant failure in the maxilla was 17.5% and 4.4% in the mandible, a difference that was significant. Vascularized free flaps were associated with the lowest rate of implant failure. Radiation dose: Radiation doses lower than 45 Gy were associated with the lowest rate of implant failure, with 5% being reported at higher doses. Delay of radiation treatment to implant placement: All implant failures occurred within 36 months after treatment. Timing of implant failure: No failures occurred within one month, 3.1% failed within the first month and 0.8% failed after 1 year.
Discussion:Based on this study, the timing of implant placement (pre- or post-therapy)is not linked to a significant difference in implant failure rate, however significantly better outcomes were noted in the mandible.
Topic: Radiation
Title:Time interval after radiotherapy and dental implant failure: systematic review of observational studies and meta-analysis
Source:Clinical implant dentistry 2013;1-10
Type:Systematic Review
Rating:Good
Keywords:dental implants, meta-analysis, osseointegration, osteoradionecrosis, radiotherapy
Purpose: To compare the risk of failure of dental implants placed within 6 and 12 months after the end of radiotherapy versus the risk of those implants placed after 12 months from the end of radiotherapy.
Materials and method
Four electronic databases were searched for articles published until February 2013 without language restriction: Lilacs, Medline, Scopus and the Cochrane Central Register of Controlled Trials. Two reviewers independently assessed the eligibility criteria and extracted data. Meta-analysis was performed.
Results:Overall 3,749 observational studies were identified. After the screening of titles and abstracts, 236 publications were selected, and finally 10 articles were included in the analysis. The Relative Risk of failure (1.34) was higher in individuals who had dental implants installed between 6 and 12 months after receiving radiotherapy.
Discussion:The main finding was that placement of dental implants between 6 and 12 months postradiotherapy was associated with 34% higher risk of failure. This is statistically significant and clinically relevant. Literature suggests that patients treated with radiation doses exceeding 50 Gray Units (Gy) are at increased risk of failure of osseointegration because of the loss of ability to repair and neovascularize the irradiated bone. Hyperbaric Oxygen therapy (HBO) reduces the risk of failure of the implant because it increases the number of capillaries and fibroblasts. However, this was not observed in this review which agrees with results of Esposito who found that HBO is not essential.
Conclusion: Minimum waiting period of 6 months postradiotherapy prior to dental implant placement is unlikely to be the most suitable, and healing periods with duration over 1 year may be beneficial.
Topic: Implants and Radiotherapy
Authors: Atanásio Pitorro TE, de Araújo Reis NT, Paranhos LR, Ferreira Soares PB
Title: Survival of Dental Implants Placed Pre-Radiotherapy Versus Post-Radiotherapy in Native Bone: A Systematic Review
Source: Int J Oral Maxillofac Implants. 2022 Nov-Dec;37(6):1100-1109
DOI: 10.11607/jomi.9756
Type: Systematic Review
Keywords: Head and neck cancer, radiotherapy, dental implant, survival rate,
Background: Ionizing radiation as a treatment for head and neck cancer can cause irreversible hypervascularity, hypoxia and hypocellularity of the bone, endothelium, periosteum and connective tissue, negatively affecting bone turnover and healing ultimately altering the osseointegration of dental implants.
Purpose: The purpose is to quantify the survival rate of implants placed pre-radiotherapy and post-radiotherapy compared to no radiotherapy in patients with head and neck cancer.
Material and methods: Observational studies, randomized controlled trials, case series and quasi-experimental studies related to the survival rate of dental implants in patients with a history of head and neck cancer receiving radiotherapy were manually and electronically searched from 10 databases. The risk of bias was assessed using the Joanna Briggs Institute critical appraisal tool.
Results: Sixteen studies were included in this study, 4 of which had a high risk of bias, 7 with a moderate risk of bias and 5 studies which had a low risk of bias. Results revealed that there was a median 60-month follow-up period. There is an 80-100% dental implant survival rate when placed post-radiotherapy, 89.4-97% survival rate when placed pre-radiotherapy and 92.2-100% survival rate when placed without radiotherapy. One study showed a statistically higher survival rate for implants placed without radiotherapy compared to implants placed post-radiotherapy. The other 15 studies showed that there was no significant difference between pre-radiotherapy, post-radiotherapy and no radiotherapy. However, all studies showed that there is a higher survival rate of implants in patients who did not receive radiotherapy.
Conclusions: In conclusion, dental implants surgically placed pre-radiotherapy and post-radiotherapy have high survival rates despite the effects of ionizing radiation on peri-implant tissue. Although the survival rates of implants placed in patients receiving radiotherapy are lower in patients that never received radiotherapy, it was not found to be statistically significant and can be considered a relatively safe procedure to help improve the quality of life of these patients. More research with heterogeneity in the survival rates, less bias and better study designs is required.
Other disorders involving bone or soft tissue
Topic: cemento-osseous dysplasia, cemento-ossifying fibroma
Author: Gerlach RC, Dixon DR, Goskel T, Castle JT, Henry WA
Title: Case presentation of florid cemento-osseous dysplasia with concomitant cemento-ossifying fibroma discovered during implant explantation
Source: Oral Surg Oral Med Oral Pathol Oral Radiol 2013 Mar;115(3):e44-52
DOI: 10.1016/j.oooo.2012.05.020
Type: Case report
Keywords: implant explantation, florid cemento-osseous dysplasia, cemento-ossifying fibroma
Purpose: This case report details a unique manifestation of florid cemento-osseous dysplasia (FCOD) and cemento-ossifying fibroma (COF) associated with implant failure within the same patient
Methods: 39-year-old African American female whose medical history was positive for diabetes, hypertension, anxiety, and NKDA. Symptomatic mandibular right first molar with a large periapical radiolucency. Initial endodontic therapy attempted, and when symptoms were not relieved, tooth was extracted with ridge preservation. After 6 months, #30 extraction sited demonstrated irregular radiopaque progression within the previous radiolucent lesion but was interpreted as a “healing phase”. Implant of 5×13 mm was placed in site #30 and restored.
After 26 months of function, patient returned with mobility on #30 implant, along with a buccal inflammation (of 1×2 cm) and tenderness adjacent to the implant. Radiographs showed multiple, mixed radiolucent/radiopaque lesions circumscribed around the apices of the mandibular anterior and posterior teeth. The lesions were evident on a series of panoramic radiographs dating back to 2007. From the panorex in 2007, a large periapical radiolucency can be seen at the apices of #30, which persisted after the extraction. It progressively increased in radiopacity and became a circumscribed, mixed radiolucent/radiopaque. CBCT scan from 2010 showed a buccal expansile lesion with an inner radiolucent core surrounded by a thin sclerotic border adjacent to irregular, dense, radiopaque bone surrounding implant #30. Other small regions of mixed radiolucent/radiopaque can also be seen in proximity to the implant. The inferior alveolar nerve canal has been displaced to the lingual aspect of the body of the mandible. Patient was scheduled for surgery to enucleate the lesion and remove the implant with differential diagnosis of FCOD, COF, giant-cell lesion, and odontogenic tumor. All specimens were submitted to pathology for histological examination for final diagnosis.
Results: This case report details a diagnosis of 2 distinct disease entities associated with the implant site, FCOD and COF of the mandibles. Based on radiographic evidence and surgical gross examination, a definitive diagnosis of FLCOD was made. A more recent, rapidly expansile, osseous lesion was also diagnosed as COD based on clinical, surgical, radiographic, and histologic evidence. Both diagnoses were verified after biopsy and removal of the previously osseointergrated implant following postinsertion failure by fibrous encapsulation.
Discussion: Before implant therapy, it is essential to conduct a thorough radiographic evaluation of any dental arch with suspected bony lesions to prevent implant failure, as a diagnosis of any COD lesion is considered a contraindication. Any radiolucent lesion should be suspected as a possible early lesion of FLCOD if accompanied by other mixed radiolucent/radiopaque lesions within either dental arch (primarily the mandibular arch). Once diagnosed, treatment considerations include frequent follow-ups, annual radiographic surveys, and aggressive preventive measures to prevent further tooth loss or need for surgery. Tooth-borne prostheses such as a fixed or removable partial denture that are the recommended procedures instead of implant therapy.
Topic: Treatment planning
Title: Branemark System Implants and Rare Disorders: a Report of Six Cases
Source: Int J Perio Rest Dent. 2013; 33:139-48
DOI: 10.11607/prd.1429
Type: Case Report
Reviewer: Maggie Weber
Rating: Good
Keywords: dental implant; rare disorders; langerhan; hypophosphatemia; osteogenesis; dentinogenesis
Purpose: to describe the outcome of oral implant treatment in patients suffering from rare disorders.
Background:
- X linked hypophosphatemia (XLH)
- X linked dominant osteomalacia effecting 1:20,000
- Clinical features: growth retardation, limb deformities, joint pain, osteoarthritis
- Oral manifestations: loss of teeth due to abscess without evident caries
- Langerhans Cell Histiocytosis
- Common term for: eosinophilic granuloma, Hand-Shuller-Christian disease, Letterer-Siwe disease effecting 9:1,000,000
- Oral manifestations: soft tissue ulcers, gingival bleeding, pain, periodontal damage, tooth mobility and loss
- Osteogenesis Imperfecta/Brittle Bone Disease
- Genetic disorder effecting 1:20,000
- Clinical features: bone fractures without trauma, hearing loss
- Oral manifestations: worn enamel, defective dentin, small/calcified pulp chambers2
Discussion:
X linked hypophosphatemia (XLH) case reports
- Patient 1: generalized tooth loss
- 4 implants placed (2 anterior mandible and two central maxillary) and follow up of 50 months
- After implant placement healing time was 1 year before abutments connected due to mobility
- 3 unit fixed prosthesis was received 2 years after initial implant placement
- Bone response at 50 months followup in all 4 implants was unremarkable
- Patient 2: generalized tooth loss
- 4 implants placed (maxillary anterior) and followup of 20 months
- After implant placement healing time was 1 year prior to abutment connection
- Fixed prosthesis was delivered a year after implant placement
- Bone response was unremarkable 20 months followup
- Patient 3: complete edentulism
- 6 implants placed in maxilla and 4 implants placed in mandible
- After implants healing time of 1 year in maxilla and 10 months in mandible, abutments were connected and prosthesis delivered
- Bone response around all 10 implants was unremarkable at 19 and 22 month followup
Langerhans Cell Histiocytosis case reports
- Patient 1: generalized tooth loss
- 4 implants placed in mandible
- Healing period of 2.5 months prior to abutment connection with 2, 3-unit fixed prostheses
- Bone response at 5 years was unremarkable
- Patient 2: complete edentulism (minus wisdom teeth)
- 4 implants placed in maxilla and 4 in mandible, wisdom teeth extracted
- 6 months of healing time prior to abutment connection and 8-unit fixed prostheses
- Bone response at 15 years was unremarkable
Osteogenesis Imperfecta
- Patient 1: edentulous
- 6 implants placed in mandible
- After 5.5 months of healing, abutments connected
- Bone response at 4 years was not stable
Conclusion:
In X-lined hypophosphatemia patients, all 18 implants place were successfully in function after 5 years with good bone response although healing time was longer than normal. Results were similar in patients with Langerhans cell histiocytosis.
In osteogenesis imperfecta, bone resorption was seen at follow-up appointments which may or may not be a result of the disease.
Topic: Other disorders involving bone or soft tissue
Author:Strietzel, FP., et al.
Title: Implants in patients with oral manifestations of autoimmune or muco-cutaneous diseases – A systematic review
Source: Journal section: Medically compromised patients in Dentistry doi:10.4317/medoral.22786
Purpose: To study implant survival rates in patients with oral manifestations of systemic autoimmune (oral Lichen planus (oLp), Pemphigus (Pe)), muco-cutaneous (Epidermolysis bullosa (EB)), autoimmune multisystemic rheumatic diseases (Sjögren ́s syndrome (SjS), systemic Lupus erythematosus (sLE), or systemic Sclerosis (sSc)).
Methods: Systematic literature review of studies published between 1980 and August 2018 in English language using (PubMed/Medline, Embase) using MESH and search term combinations, reporting on dental implant prosthetic rehabilitation of patients with oLp, Pe, EB, SjS, sLE, sSc, study design, age, gender, follow-up period (≥ 12 months), implant survival rate. Implant-related weighed mean values of implant survival rate (wmSR) were calculated.
Results: After a mean follow-up period (mfp) of 44.6 months, a wmSR of 98.3 % was calculated from data published for patients with oLp (100 patients with 302 implants). Data of 27 patients (152 implants) with EB revealed wmSR of 98.7 % following mfp of 32.6 months. For 71 patients (272 implants) with SjS, wmSR was 94.2 % follow- ing a mfp of 45.2 months, and for 6 patients (44 implants) with sSc, wmSR was 97.7 % after mfp of 37.5 months. One case report on one patient each with Pe (two implants) as well as sLE (6 implants) showed 100 % SR following at least 24 months.
Discussion: Gingiva and other oral tissues may exhibit several pathologic phenomena as symptoms or manifestations of systemic diseases, requiring further diagnostic and interdisciplinary treatment. Guidelines regarding implant treatment of patients with oLp, Pe, EB, SjS, sLE or sSc do not exist . Implant survival rates of patients affected are comparable to those of healthy patients.
Topic: Anticoagulants
Title: What influence do anticoagulants have on oral implant therapy? A systematic review
Source: Clin Oral Implants Res. 2009 Sep;20 Suppl 4:96-106
DOI: 10.1111/j.1600-0501.2009.01770.x
Type: Systematic Review
keywords: anticoagulant therapy, bisphosphonates, coated implants, oral implants, osteonecrosis
Purpose:
- Assess the risks (both thromboembolic and bleeding) of an Oral Anticoagulation Therapy (OAT) patient undergoing implant therapy
- Provide a management protocol to patients under OAT undergoing implant therapy.
Methods:
- PICO question
- In patients with OAT what is the risk of bleeding complications when dental implants are placed, and OAT is not discontinued?
- In patients with OAT what is the risk of a thromboembolic even when dental implants are placed in and OAT is discontinued?
- Final selection was based on clinical trials, prospective and retrospective studies only
Results:
- 19 studies identified that reported outcomes of oral surgery procedures, 9 RCTs, 9 prospective studies.
- In all studies the INR was in the therapeutic range
- In 8 studies: Two protocols are compared: Discontinuation of OAT 2-4 days before surgery and Continuation of therapy. Results from these showed no difference between the two groups and all bleeding events were controlled with local hemostatic measures and no thrombolytic events reported.
- 8 studies where different hemostatic treatments were implemented. Tranexamic acid mouthwashes, gelatin sponges and cellulose gauzes were effective in controlling postoperative bleeding.
- 3 case reports describing INR and bleeding risks, the OAT medication was not altered, and hemostatic agents were used, but no correlation was found with INR ranges.
- The only evidence-based recommendation was from the American College of Chest Physicians and Guidelines from Oral Medicine that were similar:
- Patients within therapeutic INR range less than 3.5 warfarin should not be modified for simple extractions or minor surgical procedures.
- If INR is on the high end of the scale, then more complicated surgeries may present an exception to the previous rule
- Greater than 3.5 should be sent to physician for adjustment before any invasive procedures.
Discussion: This study does not suggest a higher occurrence of perioperative bleeding when appropriate hemostatic measurements were taken or when different hemostatic agents were used. The placement of implants should be considered comparable or less traumatic than the extraction of three teeth assuming no harvesting of autogenous bone grafts are necessary or needing preparation outside of the bony envelope; and OAT is not a contraindication for dental implants.
Topic: Medical Overview
Title: Risk of bleeding after dentoalveolar surgery in patients taking anticoagulants
Source: British Journal of Oral and Maxillofacial Surgery 52 (2014) e15–e19
DOI:
Type: Retrospective Study
Keywords: Haemorrhage; Tooth extraction; Apicectomy; Dental implantation; Aspirin; Acenocoumarol
Purpose: Academic Centre for Dentistry Amsterdam (ACTA) guidelines were evaluated to find out whether these procedures led to increased postoperative bleeding. The study compared the incidence in patients taking anticoagulants with that in a group of patients who were not taking them.
Methods: The study involved 206 patients who were referred to the Department of Oral and Maxillofacial Surgery of the University Medical Center Groningen, the Netherlands, for dentoalveolar operations that met the ACTA guidelines – which are:
- Maximum of 3 extractions, apicectomies, or placement of implants at the same time.
The type of surgery required were divided into 4 categories: surgical extractions, non-surgical extractions, apicectomies, and placement of implants. 103 patients were taking oral anticoagulants and 103 were not.
Patients were given a local anesthetic (4% articaine with 1/100 000 epinephrine). Procedures were as atraumatic as possible, and wounds were sutured. Post-op instructions were given verbally and in a written format to apply compression with gauze for 30 min immediately post-op. no patient was allowed to leave the hospital until bleeding stopped and instructions to call the OMFS dept. if bleeding did not stop after 30 min were given.
Two types of post-op bleeding were defined. If patient came to the hospital because bleeding could not be stopped at home, it was scored as severe. During a one-week interval patients had follow ups and were asked if they had bleeding that stopped by compression with gauze and scored as mild.
Results:
- Episodes of bleeding were most common in patients who had had surgical extractions while they were taking anticoagulants, but no significant difference was found between this group and the control.
- No patient had a severe postoperative bleeding.
- Control group had fewer mild bleeds than the anticoagulant group.
Conclusion: The study concluded that that dentoalveolar surgery is safe in patients being treated with anticoagulants provided that the conditions described in the ACTA guidelines are met.
Topic: Anticoagulants
Title: Gomez-Moreno G, et al. Dental implant surgery in patients in treatment with the anticoagulant oral rivaroxaban. (xarelto)
Source: Clin Oral Imp Res. 2016; 27:730-733
DOI: 10.1111/clr.12653
Type: Clinical
Keywords: bleeding; dental implants; rivaroxaban; tranexamic acid
Purpose:The purpose of this study was to evaluate the incidence of bleeding complications after dental implant placement in patients in treatment by the anticoagulant oral rivaroxaban without interrupting its administration or modifying dosage.
Methods:
- 57 patients were divided into two groups: 18 had been in treatment by rivaroxaban for over 6 months before implant surgery and a control group consisted of 39 healthy subjects.
- All subjects received dental implants in different positions, without interrupting or modifying rivaroxaban dosage.
- Patients were treated in an outpatient setting. Non-absorbable sutures were used, and all patients were given gauze impregnated with tranexamic acid 5% (Lysteda), to bite on for 30–60 min. Afterward, the patient was examined again to ensure that hemorrhaging had stopped. When this had been established, the patient was given a packet of sterile gauzes and an ampoule of tranexamic acid and sent home.
- All patients were instructed to apply external ice packs to the surgical area for 6–8 h post- operatively. Avoid mouthwashes for the first 24 h after surgery, avoid aspiration movement, manipulation of the surgical area and to avoid tongue contact with the area.
- Patients carrying RPD not to wear their dentures for 2–3 weeks after implant surgery.
Results:
- One rivaroxaban patient presented moderate bleeding the day after surgery
- Two control patients presented moderate bleeding the day after and on the second day.
- Bleeding was managed with gauzes impregnated with tranexamic acid.
- No statistically significant differences
(P = 0.688) were found in relation to bleeding episodes between the groups, with a relative risk = 0.919 based on the pooled groups and 95% confidence interval of 0.078–10.844
Discussion:
- In the present study, implant surgery was performed in patients with normal renal function without interrupting or modifying rivaroxaban doses, applying local hemostasis that consisted of non-absorbable sutures, and compression with sterile gauzes soaked in 5% tranexamic acid in the surgical area for 30– 60 min; no significant differences were found between rivaroxaban patients and healthy control subjects.
- Only one rivaroxaban patient presented moderate bleeding the day after surgery, which was brought under control by applying gauze soaked in tranexamic acid solution; in this case, the patient reported that he had played some sport that morning that had coincided with the bleeding episode.
- The local application of tranexamic acid has been shown to stabilize clot formation in various oral surgical settings.
Conclusion: The present study found no statistically significant difference in the number of bleeding complications between rivaroxaban patients and a systemically healthy control group. Although the study had a small patient sample, this suggests that dental implant surgery in patients in treatment by the anticoagulant oral rivaroxaban can be performed safely in an outpatient setting applying local hemostatic measures; there is no need to interrupt or modify the coagulant dose.
Other medications Issues
Topic: Other medications
Title: Intake of Proton Pump Inhibitors is Associated with an Increased Risk of Dental Implant Failure
Source: Int J Oral Maxillofac Implants 2017 Sept/Oct;32(5): 1097-1102
DOI: 10.11607/jomi.5662
Type: retrospective cohort study, consecutively treated between 1980 and 2014
Keywords:Meds and dental implant failure
Purpose: To investigate the association between the intake of proton pump inhibitors (PPIs) and the risk of dental implant failure.
Methods: Modern endosseous dental implants with cylindrical or conical design were included, and only complete cases were considered; ie, only those implants with information available for all variables measured were included in the regression model analysis. Zygomatic implants and implants detected in radiographies but without basic information about them in the patients’ files were excluded from the study. Implant- and patient-related data were collected. Multilevel mixed-effects parametric survival analysis was used to test the association between PPI exposure (predictor variable) and risk of implant failure (outcome variable), adjusting for several potential confounders.
Results: A total of 3,559 implants were placed in 999 patients, with 178 implants reported as failures. The implant failure rates were 12.0% (30/250) for PPI users and 4.5% (148/3,309) for nonusers. A total of 45 out of 178 (25.3%) failed implants were lost up to abutment connection (6 in PPI users, 39 in nonusers), with an early-to-late failure ratio of 0.34:1. The intake of PPIs was shown to have a statistically significant negative effect for implant survival rate (HR 2.811; 95% CI: 1.139 to 6.937; P = .025). Bruxism, smoking, implant length, prophylactic antibiotic regimen, and implant location were also identified as factors with a statistically significant effect on the implant survival rate.
Discussion: This study suggests that the intake of PPIs may be associated with an increased risk of dental implant failure.
Authors: Wu X, Al-Abedalla K, Abi-Nader S, Daniel NG, Nicolau B, Tamimi F.
Title: Proton Pump Inhibitors and the Risk of Osseointegrated Dental Implant Failure: A Cohort Study.
Source: Clin Implant Dent Relat Res. 2017 Apr;19(2):222-232.
DOI: 10.1111/cid.12455.
Type: Retrospective Cohort Study
Keywords: epidemiology, medical devices, multilevel, osseointegrated implants, proton pump inhibitor
Background:
- PPI (Omeprazole, Lansoprazole, etc) are used to treat + prevent gastrointestinal acid-related conditions (peptic ulcer, GERD, dyspepsia, helicobacter pylori infections, eosinophilic esophagitis,
- gastrinomas, and stress gastritis.
Purpose: To determine the effect of proton pump inhibitors (PPI) on the failure of osseointegrated implants
Material and methods:
- Total of 799 patients were included in the study in Canada
- 133 osseointegrated Nobel TiUnite implants in 58 patients that take PPI
- 1640 osseointegrated Nobel TiUnite
- Kaplan-Meier estimator used to describe the hazard function of dental implant failure due to PPI use.
Results:
- 1,711 implants survived and 62 implants failure –> overall 96.5% implant survival rate
- 8% implant failure rate in pts that take PPI vs 3.2% failure rate in patients that don’t take PPI
- Smoking is associated with an increased risk of implant failure
- Regular NSAID use increase risk of implant failure HR: 2.47
Discussion
- PPI is associated with higher implant failure rate with a hazard ratio 2.73
- Mechanism of action:
- suppress gastric acidity by irreversibly inhibiting function of proton pump (H+/K+ ATPase) in the membranes of parietal gastric cells –> inhibit gastric acid secretions.
- BUT H+/K+ ATPase are also found on the plasma membrane of osteoclasts.
- Proton pump inhibition of osteoclast decrease activity + disrupts bone metabolism/ turnover + osseointegration.
- Increases pH in small intestine which reduces Ca 2+ absorption + altered calcium homeostasis –>decreases bone mineral density.
- Prolonged PPI use decrease Vit B12 serum levels which can cause hyperhomocysteinemia , impaired collagen cross linking + reduce bone strength
- Interferes with absorption + excretion of magnesium which can neg affect bone metabolism.
- Reduce expression of BMP-2, BMP-4 + CYR61 – Decrease endosteal transverse growth, increase osteoid width + decrease the ratio of bone mineral substance mass to bone mass.
- Chronic gastric acid suppression can result in hyperplasia + hypertrophy of parathyroid glands which can increase PTH levels –> can decrease bone strength + quality
- suppress gastric acidity by irreversibly inhibiting function of proton pump (H+/K+ ATPase) in the membranes of parietal gastric cells –> inhibit gastric acid secretions.
- Recommend a calcium rich diet in patients taking PPI
- Smoking can impair new bone formation, reduction Ca2 + absorption + decrease BMD transiently.
- Regular use of NSAID is usually given to patients taking PPI to prevent side effects – may affect bone metabolism by inhibiting COX-2 activity + decrease synthesis of proinflammatory prostaglandins + neg effect on endochondral ossification (Decrease bone formation)
- Patients taking PPI had the most failures btw 10 – 20 months after implant placement.
- Possible due to the inhibition of bone remodeling process around functional implants
Conclusion: This study found that PPIs usage correlated with a higher risk of osseointegrated implants failure. Clinicians should be aware of possible complications caused by PPIs prescriptions in patients undergoing treatments with osseointegrated dental implants.
Topic: Implant failure associated with intake of SSRI
Author: Chrcanovic B. R. et al.
Title: Is the intake of selective serotonin reuptake inhibitors associated with an increased risk of dental implant failure?
Source: International Association of Oral and Maxillofacial Surgeons. Volume 46, Issue 6, June 2017, Pages 782-788.
DOI: 10.1016/j.ijom.2017.01.016
Keywords: dental implant; implant failure; multilevel mixed-effects parametric survival analysis; multivariate generalized estimating equation analysis; selective serotonin reuptake inhibitors.
Purpose: To investigate the association between the intake of SSRIs and the risk of dental implant failure.
Methods:
- Retrospective cohort study.
- Patients treated with implant-supported prostheses between 1980 and 2014 at one specialist clinic.
- Included patients taking only SSRIs and no other medication and not present any other systemic condition.
- All patients had to have taken prophylactic antibiotics for implant surgery.
- All modern endosseous dental implants with a cylindrical or conical design only.
- Zygomatic implants were not included in the study, nor were implants detected in radiographs without basic information about them in the patient’s files.
- An implant was considered a failure in the presence of signs and symptoms that led to implant removal, lack or loss of osseointegration, implant mobility, continuous pain, advanced marginal bone loss, and refractory infection.
- Total of 931 implants placed in 300 patients were included in the study.
- 460 implants were placed in 145 men.
- 471 implants were placed in 155 women
- All implants were inserted with open flap surgery
Data analyses: Differences between implants placed in SSRI users and SSRI non-users were compared with:
- Student t-test or Mann–Whitney test for continuous variables.
- Wald x 2 test was used to analyze the statistical significance of each parameter within the model .
- The Akaike information criterion (AIC) was used to choose the best fit survival model .
Results:
- 35 implant failures were reported. Combined 3.75% failure rate.
- 48 implants were placed in 18 SSRI users.
- 883 implants were placed in 282 non-users.
- Follow-up from 1578 to 1717 days (SSRI users).
- Follow-up from 2804 to 2267 days (SSRI non-users).
- SSRI users implant failure was 12.5 % (6/ 48)
- SSRI non-users implant failure was 3.3% (29/883)
- Fewer implants were placed in the mandible in relation to the anterior maxilla, and fewer patients were followed up for longer periods in the SSRI user group than in the non-user group, and these differences were statistically significant.
- Table 1 screenshot.
- Intake of SSRIs, age, sex, implant diameter, or bone augmentation did not have statistically significant influence on implant failure. However, longer implants failed less than shorter implants.
4 different statistical methods were used.
- Fisher’s exact test showed a statistically significant association between the intake of SSRIs and an increased risk of implant failure. However, this test does not take into consideration the other confounders.
- Kaplan–Meier analysis showed a statistically significant difference in the cumulative survival rate between SSRI users and non-users. Although this test considers the factor time, it does not consider the influence of the other variables .
- The multivariate GEE method did not find a statistically significant association between the intake of SSRIs and an increased risk of implant failure.
- The multilevel mixed-effects parametric survival analysis showed no statistically significant association between the intake of SSRIs and a higher risk of dental implant failure.
Discussion:
- Influence of the follow-up time on the failure rate.
- Lower risk of failure with a longer follow-up, may be connected to that 31.4% of the implants were lost prior to the abutment connection procedure and 51.4% up to 1 year after surgery.
- This study showed no statistically significant association between the intake of SSRIs and a higher risk of dental implant failure.
Conclusion- the intake of SSRIs may not be associated with an increased risk of dental implant failure.
Topic: Effect of medications on implants
Author: Chappuis V, Avila‐Ortiz G, Araújo MG, Monje A.
Title: Medication-related dental implant failure: Systematic review and meta-analysis Source: Clinical oral implants research. 2018 Oct; 29:55-68.
DOI: 10.1111/clr.13137
Type: Systematic review and meta-analysis
Keywords: Dental implant, failure, Medication, biologic complications.
Purpose: Evaluate the effect of the intake of different systemic drugs on implant failure rate.
Methods:
- The review was conducted according to the guidelines of the Preferred Reporting Items of Systematic Reviews and Meta-analyses (PRISMA) statement.
- The primary outcome was implant failure (IF) while the secondary outcomes were biological and mechanical causes associated with IF.
- PECO questions were P: Human adults receiving implant supported prosthesis, E: regular intake of systemic drugs that may affect bone metabolism, C: Individuals not taking relevant medications, O: Dental implant failure (primary) biological and mechanical complication (secondary).
- The study included relative Prospective or retrospective cohort, case–control, cross-sectional, or randomized controlled trials in any language.
- Electronic and manual literature searches were conducted by two independent authors in multiple databases for all relevant studies published up to May 2017.
Results:
- Initial search of databases yielded 430 articles out of which 40 full text articles were assessed the 17 articles were selected for qualitative assessment. Five studies evaluated the use of nonsteroidal anti-inflammatory drugs (NSAIDs), two on proton pump inhibitors (PPIs), seven on oral bisphosphonates (BPs), one on anti-hypertensives (AHTNs) and two on selective serotonin reuptake inhibitors (SSRIs).
- Patients receiving PPIs and SSRIs showed higher incidence of IF compared to control groups while no meta-analysis could be conducted for AHTNs as only one study was included, and it showed increased survival rate of implants in patients receiving AHTNs.
- NSAIDs and BPs showed no significant results.
Discussion:
- The results from this study should be interpreted with caution and only an association relationship can be concluded, and no cause-effect relationship can be established.
- Bisphosphonate therapy could cause increased risk of osteonecrosis of the jaw as a consequence of dental extraction and other oral surgeries thus care should be taken when utilizing the results in this study and remember that the intake of intra-venous BPs is considered an absolute contraindication for implant therapy.
- A more prospective manner of investigation is recommended to control other contributing cofactors.
- Timing of implant failure is another important factor that needs to be better reported.
Topic: Implants and medical conditions
Author: Radzewski, R.,Osmola, K.
Title: Osseointegration of Dental Implants in Organ Transplant Patients Undergoing Chronic Immunosuppressive Therapy
Source: Implant Dentistry / Volume 00, Number 00 2019
DOI: 10.1097/ID.0000000000000916
Type: Clinical study
Keywords: crestal bone level, solid- organ transplantation, endosseous implant, immunosuppression
Purpose: to evaluate the effect in terms of function and esthetics, that implanto- prosthetic treatment has on patients who are subject to immunosuppressive treatment after organ transplants.
Methods: 21 patients received altogether 24 implants. The control group=15 people with 15 implants in place. The inclusion criteria were:>25 years of age, at least 1 year after organ transplant, in need of a single missing tooth replacement with titanium implant, at least one tooth missing with neighboring teeth present, suitable bone condition for implantation procedure without the need of guided bone regeneration (GBR). The exclusion criteria were: active periodontal disease, occlusion disorders, bone diseases, blood coagulation disorders, untreated dyslipidemia and smoking. An additional exclusion parameter for control group was immunosuppressive medication. After 4 months, a single crown was placed. The parameter that they evaluated was crestal bone level (CBL), using radiological and mechanical means.They measured the torque to locate the implant and the implant stability quotient. The time devoted to osseointegration was extended to 4 to 6 months. Measurements were performed twice: on the day of implantation and after the integration period.
Results: The basic measured parameter of CBL median revealed lack of significant differences between the experimental group and the control group. The only statistically significant difference in CBL was found between patients taking 1 or 2 medications.
Discussion: The results of this study showed that there is no difference in the effects of dental implant treatment between patients in the course of immunosuppressive therapy after organ transplantation and the control group of healthy people, and successful osseointegration concerned 100% implants. Contemporary medications exert considerably lower influence on osseointegration and are less toxic to bone and solid organs of the patient.
Conclusion: Patients with organ transplants can safely and effectively undergo dental implant treatment.
Topic: risk for DI failure- medication , Allergy to Penicillin
Authors: Zahra B, Nicholas B, Geoffrey R, Dina Z, Janal MN, Stuart F.
Title: Dental implant failure rates in patients with self-reported allergy to penicillin
Source: Clin Implant Dent Relat Res. 2022 Jun;24(3):301-306
DOI: 10.1111/cid.13082
Type: retrospective
Keywords: allergy, dental implant, penicillin
Purpose: To compare DI failure rates in pts rx’ed amoxicillin with pts who report a penicillin allergy
Material and methods:
- Chart review conducted
- Included pts w 1+ DI placed by dentists in postgrad specialty programs at New York University College of Dentistry with follow-ups at 1-2 wk and 1+ year post-DI placement
- Excluded medically-compromised pts
Results:
- DI failure rates
- Overall failure rate: 12.9%; NSSD with gender (13.2% men and 12.6% women)
- Pts w/o a reported PCN allergy: 8.4%
- Pts reporting allergy: 17.1% (SSD)
- OR: 2.22
- Clindamycin + azithromycin were major abx prescribed to pts reporting PCN allergy; both had elevated failure rates.
- DI failure relative to that with amoxicillin
- Clindamycin: OR= 2.9
- Any other abx tx: OR= 2.77
- Most failures occurred before 6mo in pts w reported allergy and after 12mo in pts w/o allergy
Conclusions:
- Study show a sig relationship between pts with reported PCN allergy and DI failure.
- Routine testing for those who report an allergy may be advised.
- Advise studying those with true allergies
Topic: Medication and implant failure
Authors: Carr AB, Revuru VS, Lohse CM
Title: Risk of Dental Implant Failure Associated With Medication Use
Source: J Prosthodont. 2019 Aug;28(7):743-749
DOI: 10.1111/jopr.12773
Type: Clinical
Keywords: medication, risk, implant failure rate
Purpose: to identify risk of implant failure related to medication use
Material and methods:
- 6384 pts receiving dental implants at Mayo Clinic between Oct 1983 to Dec 2014
- Demographics included age at time of first implant placement, sex, race/ethnicity, and era of first implantation (1983-2000 and 2001-2014)
- Analysis of medications divided into aspirin and 6 drug classes
- Anticonvulsants
- Bisphosphonates (Oral)
- Bisphosphonates (IV)
- Antihypertensives
- Antidepressants
- Corticosteroids
Results:
- 6358 patients analyzed
- 713 pts had implant failure, median of 0.6 year after 1st implant placement
- 5645 pts implants survived, median 5.8 years
- Medication use significantly associated with age
- Some meds sig assoc with sex (women and antidepressants, men and aspirin)
- Era of implantation was strongest predictor of implant failure
- Implants placed between 2001 – 2014 sig less implant failure than 1983 – 2000
- Use of multiple medications with and without aspirin had no sig influence on implant failure
- Each 10 year increase in age was assoc w/ 6% increased risk of implant failure
- Men were 22% more likely to have implant failure (vs women)
- Corticosteroids assoc with reduced risk of implant failure
- No meds started after implant placement was assoc with increased risk of implant failure
Discussion
| This study | Other studies | |
| Bisphosphonates | NSD risk of implant failure among pts receiving oral BP, IV BP, and no BP | Mixed evidence on risk of implant failure |
| Antihypertensives | NSD | Wu reduced risk of implant failure rates in pts taking antihypertensive meds |
| Antidepressants | NSD | Wu higher implant failure rate in pts using SSRI
Chrcanovic higher implant failure rate, but NSSD |
- Anticonvulsants – no diff in implant failure rate
- Corticosteroids – protective association
- PPI (not included in this study) – associated with increased risk of implant failure
Conclusion: Use of medication was not associated with an increased risk of implant failure. Corticosteroid may reduce risk of implant failure.
Topic: Implant Risk factor-medications
Authors: Carr, A., Gonzalez, R., Jia, L., Lohse, C.
Title: Relationship between Selective Serotonin Reuptake Inhibitors and Risk of Dental Implant Failure
Source: J Prosthodont. 2019 Mar;28(3):252-257
DOI: 10.1111/jopr.13015
Type: Retrospective
Keywords: Antidepressants; implant outcome; shared decision making
Purpose: To identify associations between implant failure and SSRI use.
Material and methods: Retrospective review of patient who received at least 1 dental implant in Mayo clinic between 1995 through 2014. Analyzed patient who took SSRI (6) (citalopram (Celexa), escitalopram (Lexapro, Cipralex), fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), paroxetine (Paxil, Paxil CR, Pexeva), and sertraline (Zoloft)). Statistical analysis performed.
Results:
- 3 Temporal relationship of SSRI use and implant failure:
- History of SSRI use: used concurrent with or before the date of first implant placement
- The 284 patients (5.2%) who started treatment with sertraline before the date of first implant were significantly more likely to have implant failure than patients who started a different SSRI before the date of first implant and patients with no history of SSRI use (Hazard Ratio: 1.60)
- HR: history 1 SSRI (1.08) compared to 2 or more SSRI (1.67) with implant failure rate
- Active SSRI use: use concurrent with time of first implant placement
- Active SSRI use was not significantly associated with implant failure for any of the SSRIs evaluated.
- Nearly all patients with active SSRI use were taking only 1 SSRI (98%)
- Follow-up use: initiating SSRI use after implant placement
- no significant association between SSRI use during follow-up and implant failure
Discussion:
- Only sertraline had a significant association with implant failure, and this association was evident only in patients with a history of medication use. Neither active users of sertraline nor those who began sertraline use after implant placement had significantly greater risk
- Multiple SSRIs significantly increases risk of implant failure. Compared with patients with no history of SSRI use, patients who used 2 or more SSRIs had significantly greater risk of implant failure.
Conclusions: The findings of this study shows that patients who have a history of sertraline use and are considering oral reconstruction with dental implants have a 60% greater risk of implant failure than patients with no history of sertraline use.
Periodontal disease as a risk factor for implant failure
Topic: Survival of teeth vs dental implants
Author: Guarnieri R, Di Nardo D, Di Giorgio G, Miccoli G, Testarelli L.
Title: Longevity of Teeth and Dental Implants in Patients Treated for Chronic Periodontitis Following Periodontal Maintenance Therapy in a Private Specialist Practice: A Retrospective Study with a 10-Year Follow-up.
Source: Int J Periodontics Restorative Dent. 2021 Jan-Feb;41(1):89-98.
DOI: 10.11607/prd.4674.
Type: Clinical Study
Keywords: teeth, dental implants, chronic periodontitis, periodontal maintenance
Purpose:Assess the progression of periodontal disease and the onset of peri-implant disease over a long-term period in a cohort of patients with chronic periodontitis. Assess rates of tooth and implant loss, in addition to associated risk factors.
Materials and Methods:
- 58 patients who had receive active periodontal therapy and at least 10 years of maintenance
- All patients exhibited generalized moderate-to-severe chronic periodontitis
- Active periodontal therapy included initial therapy, periodontal/implant surgery
- Primary outcomes: tooth and implant loss
- Secondary outcomes: changes in periodontal and peri-implant clinical parameters and radiographic bone levels.
Results:
- Average tooth loss during periodontal maintenance: 0.07 teeth/patient/year
- Due to periodontal reasons: 0.04 teeth/patient/year
- 78 teeth extracted (1.3/patient)
- 90% survived
- 12 implants removed from 12 patients during periodontal maintenance: 0.4 implants/patient/year
- Overall implant failure: 10.08%
- Due to biologic reasons: 9.8%
- Overall mean values of PPD, CAL, FMPS and PPD % of 1-4mm/5-6mm->6mm significantly decreased from baseline to 10 years follow-up
- Significant decrease mostly during active periodontal therapy
- Mean bone loss
- Teeth: 1.5mm
- Implants: 3.1mm
- % of implant loss in patients with vs without recurrent periodontal disease: 83.3% vs 16.7%
- Increase risk for tooth/implant loss
- Age, smoking habit, number of pockets 5-6mm and full mouth bleeding score >25%
Conclusion: Active periodontal therapy with long-term maintenance is successful in keeping the majority of periodontally compromised teeth. In those same patients, higher tendency for implant loss was found.
Topic: Risk factors for implant failures (Periodontal disease)
Authors: Safii SH, Palmer RM, Wilson RF.
Title: Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: a systematic review and meta-analysis.
Source: Clin Implant Dent Relat Res. 2010 Sep;12(3):165-74.
DOI:10.1111/j.1708-8208.2009.00162.x
Type: Review
Keywords: Bone loss, dental implants periodontitis, systematic review
Purpose: To determine the risk for implant failure and marginal bone loss around implants in patients with a history of periodontitis vs patients who are periodontally healthy
Material and methods:
- Electronic and manual search for prospective and retrospective clinical studies related to periodontal and perio-implant variables in patients with periodontitis and those who were periodontally healthy with a follow up of 3- 10 years
Results:
- 17 studies were included in the review.
- 6-11.2% implant loss in patients with history of periodontitis vs 0-3.3% in healthy patients
- 2 mm bone loss around implants in patients with history of periodontitis vs 1.7 mm bone loss in healthy patients
- Patients with a history advanced periodontitis or aggressive periodontitis had disease progression around teeth (increase PD + BOP)
- Sig association between poor plaque control + peri-implant disease
- OR 14.3 for prevalence of peri-implantitis with very poor plaque scores
- OR 2.9 for peri-implant mucositis with very poor plaque scores
Discussion:
- NSSD but more favorable implant survival rate in healthy patients vs those with a history of periodontitis
- History of periodontitis is not a contraindication for implant placement.
- Periodontally heathy patients were 3.02 times more likely to have better implant survival than previously treated periodontitis patients
- SS greater marginal bone loss in patients with a history of periodontitis vs healthy patients
- Standardized mean difference 0.61 mm
- increase susceptibility to implant failure in more progressive formed of periodontitis but not for mild periodontitis.
- Acceptable implant outcome in periodontitis patients with comprehensive supportive care+ good plaque control even in aggressive cases
Conclusion: The systematic review revealed with a moderate level of evidence that periodontitis patients exhibit a higher risk of implant failure and experience greater marginal bone loss when compared to periodontally healthy subjects.
Topic: Risk factors for DI failure- perio
Authors: Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A.
Title: Periodontitis, implant loss and peri-implantitis. A meta-analysis.
Source: Clin Oral Implants Res. 2015 Apr;26(4):e8-e16.
DOI: 10.1111/clr.12319
Type: meta-analysis
Keywords: aggressive periodontitis, chronic periodontitis, dental implants, meta-analysis peri- implantitis, periodontitis
Purpose: To evaluate perio disease as a risk factor for DI loss, peri-implantitis, peri-DI bone loss
Material and methods:
- Literature search conducted to include only prospective cohort studies that compared pts w perio to periodontally healthy pts and that reported data on DI loss, peri-implant bone level changes, or peri-implantitis
- 14 studies met inclusion criteria for meta-analysis
Results:
Meta-analysis
- Sig higher risk for DI loss in pts affected by perio had sig higher risk for DI loss (RR: 1.89), peri-DI bone loss, and peri-implantitis (RR: 2.21) vs periodontally healthy pts
Subgroup analysis
- Pts w aggressive and chronic perio had incr risk of DI loss, but incr more w aggressive (RR:4.04) vs chronic (RR. 1.59)
- For chronic perio pts, pts w severe perio had incr risk of DI loss (RR: 1.89)
Conclusions:
- Perio disease is a risk factor for DI loss, peri-implantitis, and higher levels of peri-DI bone loss
Topic: Periodontitis and Implants
Authors: Sousa V, Mardas N, Farias B, Petrie A, Needleman I, Spratt D, Donos N.
Title: A systematic review of implant outcomes in treated periodontitis patients.
Source: Clin Oral Implants Res. 2016 Jul;27(7):787-844.
DOI: 10.1111/clr.12684.
Type: Systematic Review
Keywords: clinical assessment, clinical research, clinical trials, diagnosis, epidemiology, patient centered outcomes, Periodontology, statistics
Purpose: To examine the different in outcome that treated periodontitis patient’s have with implant placement versus periodontally healthy patients.
Material and methods: 27 articles were included. The focused question was: “What are the survival and success rates (including bone-level change or bone loss) and incidence of peri-implantitis for dental implants placed in partially dentate patients who have been treated for periodontitis (‘treated periodontitis’) compared with patients without a history of clinical or radiographic evidence of periodontitis (‘non-periodontitis’)?” An electronic search took place excluding those that did not match the inclusion criteria.
Results: Implant success and survival was SS higher in periodontally healthy patients versus patient’s with a history of periodontitis. Patient’s with a history of periodontitis ihad an increase in bone loss and incidence of peri-implantitis. Patient’s who were treated for severe periodontitis had a high rate of implant loss and biologic complications. Appropriate data between studies was not available for a meta-analysis to take place.
Conclusions: In patients with a history of periodontitis, lower implant success and survival were observed, as were an increase in biologic complications compared to periodontally healthy patients. Patients with a history of severe periodontitis experienced a greater frequency of implant loss.
Topic: periodontitis
Authors: Quirynen M, Abarca M, Van Assche N, Nevins M, van Steenberghe D.
Title: Impact of supportive periodontal therapy and implant surface roughness on implant outcome in patients with a history of periodontitis
Source: J Clin Periodontol. 2007 Sep;34(9):805-15.
DOI: 10.1111/j.1600-051X.2007.01106.x.
Type: systematic review
Keywords: attachment loss, bone loss, implants, peri-implantitis, periodontitis, plaque, smoking, susceptibility
Purpose: To search for a relationship between susceptibility to periodontitis and peri-implantitis, with implant outcome as the primary outcome variable and SPT and implant surface roughness as confounding factors.
Material and methods:
- Electronic search up to June 2006
- PICO question: Is the outcome of implants in patients with a history of periodontitis similar as for periodontitis free patients, and are SPT and implant surface roughness confounding variables?”
- Outcome variables: implant loss, marginal bone, attachment level/probing depth, BOP, peri-implantitis
- Primary outcome was variable was implant outcome but special attention was paid to the impact of SPT and implant surface roughness as possible confounding factors.
Results:
- 16 papers selected: 11 prospective and 5 retrospective studies
- Early implant loss – history of periodontitis impact was negligible (0.8%)
- Late implant loss and/or marginal bone loss – higher incidence reported (mean 6.0% with 0-41% range)
- Highest for implants with very rough surface and one study where SPT was not given to patients (3x higher)
- Aggressive periodontitis patients more prone to implant loss even with minimally rough implants and SPT given.
Conclusions: Patients with a history of periodontitis can be successfully treated with minimally/moderately rough implants with regular SPT.
Authors: Levin L, Ofec R, Grossmann Y, Anner R.
Title: Periodontal disease as a risk for dental implant failure over time: a long-term historical cohort study
Source: J Clin Periodontol. 2011 Aug;38(8):732-7
DOI: 10.1111/j.1600-051X.2011.01745.x
Type: Comparative Study
Keywords: periodontitis, risk factor, smoking, implant failure
Purpose: to evaluate patient’s periodontal status and long-term implant survival rate
Material and methods:
- Prospective cohort study on 736 pts from 1996 to 2006 at a periodontal clinic
- Pt’s periodontal diagnosis classified and updated to current classification (excluded aggressive periodontitis):
- None
- Moderate chronic
- Severe chronic
- All perio pt’s underwent periodontal procedures prior to implant placement
- Other variables of interest were diabetic status, smoking status, and supportive periodontal therapy
- Cumulative survival rates calculated
Results:
- Follow up time was up to 144 mo, avg of 54 mo
- Sig correlation between periodontal status and diabetes, smoking, and SPT
- Higher proportion of diabetic/smoker/SPT pt’s observed in severe chronic periodontitis group
- Higher implant failure rates seen in severe chronic periodontitis group (5.2%)
- compared to moderate chronic periodontitis (3.3%) and healthy pts (3.0%)
- Cumulative survival rate stabilized
- Healthy pts: 0.96 around 60 mo
- Moderate chronic perio: 0.95 at 72 mo
- Severe chronic perio: 0.88 at 108 mo
- Severe chronic perio is stable up to 50 mo, but is a strong risk factor for implant failure after 50 mo
- Same with smoking, with non-significant effect up to 50 mo, and increased risk after 50 mo
Conclusion: Periodontal status and smoking are significant risk factors for late implant failures. (The risk is not constant throughout follow up, with increased risk of failure after 50 mo.)
Authors: Carra, M., Rangé, H., Swerts, P., Tuand, K., Vandamme, K., Bouchard, P.
Title: Effectiveness of implant-supported fixed partial denture in patients with history of periodontitis: A systematic review and meta-analysis
Source: J Clin Periodontol. 2022 Jun:49 Suppl 24:208-223
DOI: 10.1111/jcpe.13481
Type: Systematic Review/Meta
Keywords: bridges, implant supported fixed partial dentures, periodontitis
Purpose: Effectiveness of implant-supported fixed partial dentures (IS-FPD) in patients with history of periodontitis (HP) vs. patients with no history of periodontitis (NHP)
Material and methods: Followed PRSIMA. Electronic database (MEDLINE (through PubMed), EMBASE, Cochrane Central Library, ProQuest Dissertations and Thesis, Open Access Thesis and Dissertation, openthesis.org, OpenGrey database and ClinicalTrials.gov) search.
*Statistical definition:
Hazard ratio (HR) can be considered as an estimate of relative risk, which is the risk of an event (or of developing a disease) relative to exposure.
Relative risk (RR) is a ratio of the probability of the event occurring in the exposed group versus the control (non-exposed) group.
Results: 7 Prospective and 10 retrospective studies.
- Survival rate (hazard ratio)
- Significantly higher in the NHP group than HP group
- No SS difference between severe periodontitis and moderate periodontitis
- Reasons for implant failure
- Most frequent complication leading to implant loss was peri-implantitis
- Other reasons
- Implant fracture or trauma
- Lack/loss of osseointegration
- Implant mobility
- Pain or paresthesia
- Success rate:
- Heterogeneity in reporting
- No pooled data analysis possible
- Individual reports
- Degidi et al: 10 year prospective follow-up -> 62.6% for overall study population
- Gatti et al: 5 year prospective follow-up -> 97.9% for severe periodontitis group and 100% for moderate periodontitis or periodontally healthy
- Ormianer et al: retrospective of 9.5 years -> 90.9%
- Peri-implantitis rate:
- Patients with HP had RR of 3.3 of developing peri-implantitis over the follow-up period compared to NHP patients.
- MBL changes
- no difference in MBL between implants placed in HP and NHP patients
- Heterogeneity in reporting
Discussion:
- HP patients have a poorer long-term survival and a greater risk of peri-implantitis compared to IS-FPDs placed in NHP patients.
- No differences between the HP and NHP groups are detected for MBL changes over time
- No conclusion can be drawn on IS-FPD overall success rate
Topic: Implants and hx periodontitis
Authors: Roccuzzo A., Imber JC., Marruganti C., Salvi GE., Gamieri G., Roccuzzo M.
Title: Clinical outcomes of dental implants in patients with and without history of periodontitis: A 20-year prospective study
Source: J Clin Periodontol. 2022;49:1346–1356.
DOI: 10.1111/jcpe.13716
Type: Prospective study
Keywords: dental implants, peri-implantitis, periodontitis, supportive periodontal therapy, tooth loss
Purpose: To compare 20-year clinical outcomes of tissue-level implants placed in pts previously treated for periodontitis and in periodontally healthy pts.
Material and methods: The study population was 149 partially edentulous pts rehabilitated in a private practice setting with tissue level SLA dental implants.
- Divided into three groups:
- periodontally healthy pt (PHP)
- moderately periodontally compromised pts (mPCP)
- severely periodontally compromised pts (sPCP)
- After periodontal/implant interventions, subjects were enrolled in individualized supportive periodontal care (SPC) programs.
Results: A total of 84 pts rehabilitated with 172 implants completed the 20-year examination.
- 22 PHP, 29 mPCP and 33 sPCP subjects, corresponding to 39, 59 and 71 implants, respectively.
12 implants were removed (11 biological complications, 1 implant fracture)
- Overall implant survival rate of 93%
- 9% for PHP
- 8% for mPCP
- 1% for sPCP
FMPS and FMBS were SS difference among groups at baseline.
- At 20-years, FMPS and FMBS decreased for all groups and failed to show statistical differences at this point.
Implant loss:
- PCP compliant with SPC did not experience higher odds of implant loss compared to PHP compliant with SPC.
- PCP not compliant with SPC experienced implant loss with OR of 14.59
- In comparison PHP not compliant with SPC experienced implant loss with an OR of 8.55.
Conclusion:
PHP compliant with SPC experience fewer biological complications in the long-term than patients with a hx periodontitis. Pts with a history of periodontitis may achieve excellent implant survival if compliant with SPC. However, patients not compliant with SPC are at a significantly higher risk for biological complications and implant loss.
Topic: Periodontitis effects on implant failure
Author: Monje A, Alcoforado G, Padial-Molina M, Suarez F, Lin GH, Wang HL
Title: Generalized aggressive periodontitis as a risk factor for dental implant failure: a systematic review and meta-analysis.
Source: J Periodontol. 2014 Oct;85(10):1398-407.
DOI: 10.1902/jop.2014.140135
Type: Systematic Review
Keywords: generalized aggressive periodontitis, dental implant, failure
Purpose:
- Assess whether patients who suffer from generalized aggressive periodontitis (GAgP) have a higher implant failure rate and MBL in implant prostheses when compared with patients with chronic periodontitis (CP) and/or healthy patients (HP)
Materials and Methods:
- Electronic search
- Focus question: Do edentulous patients restored with implant-supported prostheses have a higher or similar implant survival rate (SR) and/or MBL among patients with a history of GAgP and/or HPs and/or patient with CP?
Results:
- 6 articles included: comparative prospective controlled traisl assessing implant treatment outcome in patients with GAgP compared with HP/CP
- GAgP on SR of implants
- GAgP: 83.3% to 100%
- CP: 96.4%-100%
- HP: 96.9%-100%
- When looking at failure rate
- AgP vs HP: overall risk ratio of 4.00
- AgP vs CP: overall risk ratio of 3.97
- GAgP on MBL
- HP vs CP: WMD of 0.15mm favoring CP
- HP vs GAgP: WMD -0.28mm favoring HP
- CP vs GAgP: WMD -0.43mm favoring CP
- Effect of follow-up period on SR of GAgP
- Length of follow-up period did not significantly influence the outcome in either HP vs GAgP or CP vs GAgP
Conclusion:
- Patients with a history of GAgP had similar SR when compared with CP and HP groups
- Implant placement viable in patienst with history of GAgP
- When comparing failure rates, GAgP vs HP (risk ratio 4.0) and GAgP vs CP (3.97)
- Comprehensive implant maintenance program is important
- Comprehensive implant maintenance program is important
Topic: Risk factors for implant failures (Periodontal disease)
Authors: Smith MM, Knight ET, Al-Harthi L, Leichter JW
Title: Chronic periodontitis and implant dentistry.
Source: Periodontol 2000. 2017 Jun;74(1):63-73.
DOI:10.1111/prd.12190
Type: Review
Keywords: dental implants, periodontitis, chronic periodontitis
Background:
- Short term studies show similar survival rates in patients with or without a hx of chronic periodontitis.
- Long term studies > 10 years show a sig increase incidence of peri-implant complications in patients with periodontitis.
- Poor plaque control, history of periodontitis + cigarette smoking are the strongest risk indicators for peri-implantitis
- Other factor affecting plaque accumulation + removal à design of prosthesis + excess cement
Purpose: To review the evidence that a history of periodontitis is a risk factor for implant success + survival
Discussion:
- Implants in patients with a history of periodontitis
- Limited evidence for lower success + survival of dental implants in patients with a history of periodontitis
- Evidence to support this is very weak due to different definition of success or treatment of periodontitis, study quality + design
- Nevins + Langer: >97% implant survival in patients with recalcitrant periodontitis (continued periodontal bone loss despite active management
- The main study quoted as evidence to place implants in patients with a history of periodontitis but Follow up varied including only up to 3 years
- Recent studies provide evidence that patients with a history of periodontitis have a greater risk for implant loss + peri-implantitis (min of 5 year post-op)
- Peri-implant disease is slow, chronic + cyclical similar to chronic periodontitis
- Limited evidence for lower success + survival of dental implants in patients with a history of periodontitis
- Implant survival and history of periodontitis
- Long term follow up > 9 years showed patients with a history of severe periodontitis is associated with higher implant failure rate
- Patients with severe bone loss > 30% before implant tx had sig higher rates (12%) of implant failure than those with less bone loss (3%)
- No criteria for implant removal à depends on clinician assessment of bone loss + mobility
- Risk of periimplantitis for periodontitis pts is 14 x higher compared to periodontally healthy pts.
- Deeper mean full mouth PD + greater full mouth attachment loss is associated with greater attachment loss around implants.
- Periodontally compromised patients who had at least 1 periodontal pocket of ≥ 6 mm are more likely to have a greater degree of bone loss + deeper PD at implants
- Periodontally compromised patients who did not have at least 1 periodontal pocket of ≥ 6 mm had peri-implant measurements similar to periodontally healthy patients
- Supportive peri-implant therapy for patients with a history of periodontitis:
- Lack of supportive peri-implant therapy is associated with a greater incidence of peri-implant bone loss in pt over 10 yrs
- Patients with a history of periodontitis even if they are treated and considered periodontally healthy at the outset of implant treatment may benefit from greater emphasis on self-performed plaque control + more frequent supportive peri-implant therapy recall visits
- More patients who did not adhere to their supportive peri-implant therapy required a larger number of treatment with systemic ABS and or surgery for peri-implant disease
- Patients with no structured peri-implant therapy had 77% peri-implant mucositis + 15% peri-implantitis
- Serino: even with surgical intervention + supportive peri-implant therapy 42% of implants continued to exhibit characteristics of peri-implant disease
- In patients with history of periodontitis, peri-implant bone loss is not linear + accelerated sig after 7 yr of function
- Surface roughness is suggested to be a contributing factor to peri-implant disease when surface is exposed to the oral enviro
- Protocol for Implant supportive peri-implant therapy
- No evidence to recommend optimal frequency of recall interval or regimen for prevention for peri-implant disease
- Patients treatment planned for implants should already have an established effective OHI to prevent early implant failure
- Recommends increasing antibacterial potential depending on the severity + the extent of the disease
- Smoking cessation
- Cigarette smoking is associated with a greater risk of developing peri-implant diseases + implant loss
- After 10 yr in function, approx. 1 mm greater mean radiographic peri-implant bone loss in smokers with a history of periodontitis
- Cigarette is associated with a 2.8 fold increased risk of have peri-mucositis + 10 fold increased risk of bone loss to ≥ 3 threads + a 4.6 fold increased risk of peri-implantitis
- Higher implant survival rate in those who quit smoking 1 week before + 8 weeks after implant surgery
Conclusion:
- Risk factors for destructive periodontal disease + peri-implant disease are:
- Bacterial plaque, factors that hinger plaque removal + impaired healing (ie. Smoking)
- Management of periodontally involved teeth or implants in periodontally susceptible patients relies on plaque control
- Preventative program should be based on risk assessment for each patient
Parafunction
Topic: bruxism & implants
Title: Assessment of Survival Rate of Dental Implants in Patients with Bruxism: A 5-year Retrospective Study
Source: Contemp Clin Dent. 2018 Sep; 9(Suppl 2): S278–S282.
DOI: 10.4103/ccd.ccd_258_18
Type: retrospective study
Keywords: Bruxism, decementation, dental implant
Purpose: To assess complications in dental implants in bruxism patients.
Materials/Methods:
- 5-year study including 450 patients with a total of 640 implants Ø 24 patients had bruxism habits:
- complaints of tooth grinding or tapping sound at night
- confirmation of masseter muscle hypertrophy on voluntary contraction during clinical examination
- hypersensitivity of teeth to cold air
- clicking sound in temporomandibular joint movements
- presence of masticatory muscle fatigue or stiffness in the morning
- radiographs or patients’ records were evaluated for the presence of complications such as fracture of implant, fracture of ceramic, screw loosening, screw fracture, and decementation of unit Results:
- NSSD between cement or screw retained restorations o complications were seen in 145 screw-type and 130 cemented-type fixations o absent in 260 screw-type and 242 cemented-type fixations
- in cemented type of fixation, common complications were: fracture of ceramic > decementation > fracture of implant > screw loosening > screw fracture
- common complications in screw-type fixation were: fracture of implant fracture of ceramic > decementation > screw loosening > screw fracture > fracture of implant
- SSD between complications in types of prostheses o complications were seen in 45 single crowns, 125 partial prostheses, and 105 complete prostheses
- absent in 112 single crowns, 210 partial prostheses, and 180 complete prostheses
- Survival rate of dental implants with bruxism habit was 90%-92% after 1 year, 87%-90% after 2 years, 85% after 3 years, 75% after 4 years, and 70-72% after 5 years o Survival rates were slightly higher in females, but NSSD Conclusions:
- found that the common complications were fracture of implant, fracture of ceramic/porcelain, screw loosening, screw fracture, and decementation.
- the most common complication was fracture of porcelain
- overload caused by bruxism may result in failure of implant-supported prostheses
Topic: Bruxism
Author: Chrcanovic BR, Albrektsson T, Wennerberg A.
Title: Bruxism and Dental Implants: A Meta-Analysis.
Source: Implant Dent. 2015 Oct;24(5):505-16
DOI: 10.1097/ID.0000000000000298
Type: Meta-analysis
Keywords: dental implants, bruxism, implant failure rate, meta-analysis
Purpose: To compare the survival rates of dental implants, postoperative infection, and marginal bone loss of dental implants inserted in bruxers and non-bruxing patients.
Methods:
- Implant failure was defined as the complete loss of an implant
- They were able to extract the following data: days of antibiotic prophylaxis, mouth rinse, implant healing, failed and placed implants, post-op infection, marginal bone loss, bruxism definitions, implant surfaces, jaws, type or restoration, opposing dentition.
Results:
- 10 publications in total were used for this systematic review.
- 760 implants were inserted in bruxers with 49 failures, a 6.45% failure rate
- 2989 implants were placed in non-bruxers with 109 failures, a 3.65% failure rate
- Meta-analysis- the insertion of dental implants in patients being diagnosed with bruxism affected implant failure rates, a relative risk of 2.93 was found. The insertion of implants in bruxers increases the risk of implant failure by 193% compared to non-bruxers.
- No meta-analysis was available for post-op infection, or marginal bone loss.
Discussion: Due to the limited number of published studies, this study cannot suggest that implant therapy in bruxers will affect implant failure rate. The real effect of bruxing habits on osseointegration and survival of implants is not well established.
Topic: Occlusion
Authors: Bertolini MM, Del Bel Cury AA, Pizzoloto L, Acapa IRH, Shibli JA, Bordin D.
Title: Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review.
Source: Braz Oral Res. 2019 Sep 30;33(suppl 1):e069.
DOI: 10.1590/1807-3107bor-2019.vol33.0069.
Type: Systematic Review
Keywords: Bone resorption, alveolar bone loss, peri-implantitis
Background: hypothetical mechanisms:
- Lack of PDL on implants making them less tolerable to non-axial occlusal loads
- Occlusal loads are concentration at the implant marginal bone + Excessive stress can lead to bone resorption depending on bone quality
- Microdamage theory: traumatic occlusal forces are correlated to bone microfractures + consequently
Purpose: To examine the effects of traumatic occlusion on peri-implant bone levels
Material and methods: PICO Question: does traumatic occlusal forces lead to peri-implant bone loss?
Results:4 Animal studies:
-
- Podaropoulos: controlled progressive orthodontic loading results in sig higher BIC % vs unloaded implants + NSSD in crestal bone resorption
- Ferrari: Excessive lateral static load negatively affected peri-implant bone around immediate restore implants (3.68 mm vs 0.45 mm MBL)
- Nagasawa: Degenerative changes in osseointegration and or in the bone around implants upon excessive occlusal loading + immediate loading –> no OHI
- Miyamoto: static overload-induced forces resulted in sg greater bone loss –> no OHI
- 1 human study:
- Jofre: no relationship btw max bite force + MBL for patients wearing overdenture using bar or ball attachment system
Conclusions
- May be an association between occlusal overloading + peri-implant bone loss when pathologic overload (> 12 Kg/mm^2) is applied prior to osseointegration in the absence of inflammation
- Bone homeostasis loads (< 2 kg/ mm^2) applied after osseointegration leads to higher BIC + no crestal bone bone resorption in the absence of inflammation
- Magnitude of strain below the threshold will result in bone apposition + strain above the threshold will result in bone loss
- Chvartsaid: Healing adaption theory:
- The magnitude of the trauma determines whether an implant may fail or/ and will result in marginal bone loss
- Lack of clinical and scientific evidence on the influence of traumatic occlusal forces in dental implants
Topic: risk for DI failure- occlusion
Authors: Nagasawa M, Takano R, Maeda T, Uoshima K
Title: Observation of the bone surrounding an overloaded implant in a novel rat model.
Source: Int J Oral Maxillofac Implants. 2013 Jan-Feb;28(1):109-16.
DOI: 10.11607/jomi.2388
Type: animal (rat) study
Keywords: animal experiments, bone remodeling, dental implants.
Purpose: to use an animal model to assess changes in osseointegration with early and excessive loading
Material and methods:
- Included 40 rats; 16 control and 24 experimental
- Bilateral max first and second molars were extracted,
- One-month post-ext, machined DIs were placed in both groups.
- Experimental group: abutments designed to overload DIs were placed at 2 weeks (12 rats) or 4 weeks (12 rats) post-DI placement
- No abutments placed in control group
- Animals sacrificed at various timepoints, and sections prepared for histological examination
Results:
- All controls DIs were osseointegrated
- 2 DIs failed in the group with abutments placed at 2 weeks; DIs failed btwn 10-15 post-abutment placement
- placement
Histology
Control:
- Decalcified specimens: partial osseointegration at boneimpant interface. Active bone formation adjacent to DI surface. No signs of active bone resorption around the DIs.
- 4 weeks post-placement: osseointegration widely established and bone density higher at vs 2 weeks post-placement
- Non-decalcified sections: osseointegration confirmed in, esp after 4 weeks vs 2 weeks.
Experimental:
- 5 days after overloading: active bone resorption around DIs in 2 week, vs 4 week specimens.
- 10 days after overloading: degenerative tendency of osseointegration more pronounced. Bone at the DI surface was less due active bone resorption in 2week specimens.
- 15 days: almost all osseointegration had been lost in 2week specimens. While bone formation was found around residual bone, reestablishment of osseointegration was rarely observed. Two DIs failed before 15 days.
- In the 4week specimens, a wide area of preserved osseointegration was found.
Conclusions: Loss of osseointegration was found around DIs with excessive occlusal load. First study to show possibility of loss of osseointegration in absence of infection
Topic: Occlusion
Authors: Zhou Y, Gao J, Luo L, Wang Y.
Title: Does Bruxism Contribute to Dental Implant Failure? A Systematic Review and Meta-Analysis.
Source: Clin Implant Dent Relat Res. 2016 Apr;18(2):410-20.
DOI: 10.1111/cid.12300
Type: Systematic Review
Keywords: bruxism, complication, dental implant, implant failure, teeth grinding
Purpose: To determine the relationship between bruxism and DI failure.
Material and methods: Systematic review and meta-analysis. Electronic search performed. Hand search also utilized. 7 cohort studies included that meet the inclusion criteria.
Results: Most of the studies were published within the last 10 years. 3 studies based on number of prostheses, 2 on number of patients and number of prosthesis, and 2 based on patients. 2 groups created, group a was number of prostheses based and group b was number of patients based. 445 patients were included, 81 patients had a history of bruxism in group B. 1788 prosthesis were placed in group A 509 prosthesis were in patients with a history of bruxism. Both groups showed a relationship between dental implant failure and bruxism. Bruxism and DI failure showed SS and prosthesis in bruxers had higher failure rate than nonbruxers.
- In group A Odds ratio (OR) of bruxers vs nonbruxers for all subgroups was 4.72.
- In group B OR of bruxers vs nonbruxers for all subgroups was 3.63. In all of the complications, ceramic/porcelain chipping/fracture had higher failure rates vs others. Density and strength of bite force was higher in bruxers (105N) vs nonbruxers (81N).
- Overload may cause imbalance of bone absorption and remodeling leading to biologic complications, MBLoss peri-implantitis.
- Evidence from current reviews explain that the bruxism and DI failure cause and effect relationship remains controversial.
Conclusions: This meta-analysis showed that bruxism plays a role in dental implant failure. Patients with bruxism had higher failure rates versus nonbruxers, and bruxism contributes to technical/biological complications of DIs.
Topic: occlusion
Authors: Kim Y, Oh TJ, Misch CE, Wang HL.
Title: Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale
Source: Clin Oral Implants Res. 2005 Feb;16(1):26-35.
DOI: 10.1111/j.1600-0501.2004.01067.x
Type: discussion
Keywords: dental implant, implant longevity, implant occlusion, overloading
Purpose: To discuss the importance of implant occlusion for implant longevity and to provide clinical guidelines of optimal implant occlusion and possible solutions managing complication related to implant occlusion
Discussion:
- Implant occlusion. Factors to consider –
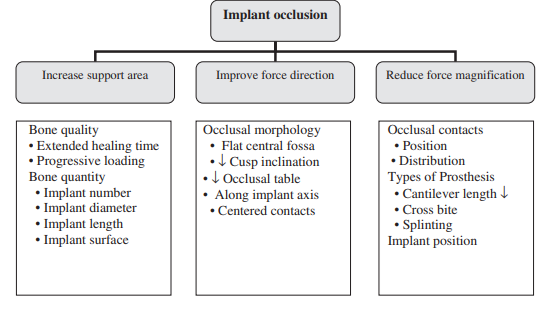
- Clinical applications
- Occlusion on full-arch fixed prostheses – bilateral balanced occlusion for opposing complete denture; group function for opposing natural dentition, mutually protected occlusion with a shallow anterior guidance also recommended; canine guidance increased potential risk of screw joint failure at canine site.
- Occlusion on overdentures – bilateral balanced occlusion with lingualized occlusion on a normal ridge; monoplane occlusion recommended for severely resorbed ridge
- Occlusion on posterior fixed prostheses – anterior guidance to reduce potential lateral force on osseointegrated implants; group function should only be utilized when anterior teeth are periodontally compromised.
- Reduced inclination of cusps, centrally oriented contacts with a 1-1.5mm flat area, narrowed occlusal table, and elimination of cantilevers have been proposed as key factors to control bend overload.
- Occlusion on single implant prosthesis – minimize occlusal force and maximize force distribution to adjacent natural teeth.

Conclusions: The objective of implant occlusion are to minimize overload on the bone-implant interface and implant prosthesis, to maintain implant load within the physiological limits of individualized occlusion, and to provide long-term stability of implants and implant prostheses. This can be accomplished by increased support area, improved force direction, and reduced for magnification.
Topic: Occlusal overload
Authors: Naert I, Duyck J, Vandamme K
Title: Occlusal overload and bone/implant loss
Source: Clin Oral Implants Res. 2012 Oct;23 Suppl 6:95-107
DOI: 10.1111/j.1600-0501.2012.02550.x
Type: Review
Keywords: peri-implant, bone loss, occlusal overload
Purpose: to review the biological consequences of overloading osseointegrated implants
Material and methods: Electronic database search to answer focus question: “what is the effect of overload compared to controls on marginal bone loss, in clinically stable implants?”
Results:
- 16 clinical and 25 animal studies were considered
- All human clinical studies were excluded due to high risk of bias, lack of sample size, missing or incomplete data, lack of evidence to support to oppose cause-effect relationship between bone loss and overload.
- 3 animals studies included.
- Uninflamed conditions
- Insignificant crestal bone resorption noted in response to supra-occlusion and confined to implant neck at 12 mo
- Supra-occlusion loading significantly increased % bone-to-implant contact and peri-implant bone density
- Inflamed conditions
- Marked radiographic peri-implant bone loss extending to implant threads at 12 mo
- Supra-occlusal loading worsened plaque-induced bone loss
Conclusion: The focused question in humans remains unanswered. In animal studies, occlusal overload did not have a negative effect on osseointegrated implants in the absence of inflammation. While in the presence of inflammation, occlusal overload significantly increased plaque-induced bone resorption.
Topic: Implant risk factors-occlusion
Authors: Chambrone, L., Chambrone, L., Lima, L.
Title: Effects of Occlusal Overload on Peri-Implant Tissue Health: A Systematic Review of Animal-Model Studies
Source: Periodontol. 2010 Oct;81(10):1367-78
DOI: 10.1902/jop.2010.100176
Type: Review
Keywords: Alveolar bone loss; dental implantation, endosseous; dental occlusion, traumatic; evidence-based dentistry; osseointegration
Purpose: To assess the clinical, radiographic, and histologic effects of excessive occlusal loads (i.e., overload) on clinically stable dental implants by questioning to what extent excessive overload may affect peri-implant tissue health.
Material and methods:
- Electronic search of MEDLINE, EMBASE, and LILACS up to January 2010.
- Studies that reported outcomes of non-splinted titanium dental implants that became susceptible to occlusal overload (OV).
- Probing depth (PD), clinical attachment level (CAL), radiographic and histologic distances from the implant base to the most coronal point of bone-to-implant contact (RDIB and DIB, respectively), and bone density (BD) were the main outcomes of interest.
- From initial search results of 347 articles only 2 were considered for full analysis; non-RCT. The follow-up periods of the study ranged from 8 to 12 months.
- Total of 10 animals and total of 80 implants were analyzed.
- Stringent levels of plaque control (i.e., implant brushing three to seven times a week and rinsing with chlorhexidine solutions)
Discussion/Results:
- When adequate plaque control was performed, there was a lack of association between OV and peri-implant tissue loss. In other words, a positive correlation between plaque accumulation and OV in terms of a significant PD increase between baseline and final measurements and DIB
- When there was no inflammation of peri-implant mucosa, the overloading of dental implants did not lead to clinical attachment loss or deepening of PDs
- Analogous to the concept of influence of traumatic occlusal forces on natural teeth.
- In the absence of dental plaque, trauma from occlusion did not contribute to the loss of periodontal structures or to the development of infrabony defects.
- In the absence of inflammation, OV led to an increase in the percentage of bone-to-implant contact and a slight reduction of marginal bone levels
- BOP was recorded in only 18% of the OV sites, although 53% of the sites showed the presence of dental plaque.
Conclusions: It is not well established if an excessive occlusal load negatively affects osseointegration when adequate plaque control is performed. OV seems to increase BD around dental implants. OV might play a key role in the development of peri-implant tissue breakdown when plaque accumulation is present.
Topic: Implant occlusion
Authors: Goldstein G., Goodacre C., Taylor T.
Title: Occlusal Schemes for Implant Restorations: Best Evidence Consensus Statement
Source: Journal of Prosthodontics, 2021, 30: 84-90.
DOI: 10.1111/jopr.13319
Type: Consensus statement
Keywords: Dental implants; occlusal schemes; occlusion; restoration.
Purpose: To review the published concepts on implant occlusal schemes and determine the effects of occlusion on implants protheses.
Material and methods: Focus question: Is there a preferred occlusal scheme for an implant retained restoration? Literature search was completed for clinical trials, RCTs, SRs, and Meta-analyses. A total of 15 articles were included in the review.
Results: Most of the identified studies reported on bone or implant loss with no definitive relationship with occlusion. With the loss of the PDL, some concern exists in the loss of proprioception leading to more susceptibility to overloading. A small number of studies suggested a potential relationship exists between implant failure and factors such as bending moments, occlusal overload, and occlusal table dimension but without strong evidence. Many studies exist reporting on implant complications. However, very few articles report on the occlusal scheme utilized in the restoration. Examining failing implants retrospectively is also problematic, as similar to teeth, causation cannot be proved, and the original occlusal scheme cannot be confirmed with certainty. Overall, there is a lack of evidence supporting one occlusal scheme over another when restoring implants.
Conclusion: There is a lack of evidence supporting an occlusal scheme to utilize with implant restorations. The planned occlusal scheme may mimic that used for tooth or mucosal supported prostheses until compelling evidence may dictate otherwise.
Age at Placement (growth)
Topic: Age
Authors: Cronin RJ Jr, Oesterle LJ
Title: Implant use in growing patients. Treatment planning concerns..
Source: Dent Clin North Am 1998;42(1):1-34.
Type: Discussion article:
Keywords: age, growth, wrist
Discussion article:
- Maxillary growth: the midface grows in a downward and forward direction relative to the anterior cranial face. Maxillary growth occurs as a result of both passive displacement and enlargement.
- The average size of the dental arches is generally greater in males than in females. Female growth is nearly completed by age 15 and males growing is longer (age 17 to 19) and at a greater rate.
- Tooth eruption and alveolar growth must be viewed as a negative factor in the placement of DI.
- Implants in boys should be delayed longer than in adolescent girls.
- The increase of alveolar height continue with eruption of the permanent incisors
- The mandible grows downward and forward.
- The mandible grows in length by growth at the condyle and ramus.
- To accommodate posterior tooth eruption, the body of the mandible increases in length by resorption on the anterior aspect of the mandible and deposition on its posterior aspect.
- As the mandible increases in length, it also increases in posterior width because of its V shape.
- Girls generally erupt their teeth 2y earlier than boys.
- Generally when the girls start menstruation, their growth is nearly complete. By age 15, most girls have nearly completed their growth, where areas many boys continue to grow into their early 20’s.
- The longer growth period for males results in more prominent lower jaw and straighter profile seen in males.
- There is no totally reliable indicator as to when growth has ceased. In fact long term studies indicate that growth never stops but continuous throughout life in the same direction as in adolescence but at a much reduce rate.
- Long bone growth, particularly in the bones in the hand and wrist, is an indicator commonly used to male an educated guess of the status growth of the pt.
Topic: Dental implants and children
Title: Osseointegrated dental implants in growing children: a literature review.
Source:. J Oral Implantol 2014. Oct;40(5):627-31.
DOI: 10.1563/AAID-JOI-D-11-00186
Type: review
Keywords: osseointegration; dental implants; children
Purpose : to review current literature of placing dental implants in young patients and discuss potential risks involved placing implants in jaws that are still developing.
Discussion: Two primary concerns: If implants are present during several years of facial growth, do they face a danger of becoming embedded, relocated, or displaced as the jaws grow? Second concern is the effect of prosthesis on growth. Implants cannot participate in maxillary growth due to behaving similar to ankylosed teeth leading to unpredictable implant dislocations or maxillary growth disturbances. The maxilla resorbs at the nasal floor and the anterior surface leading to implant dislocations in the vertical and anteroposterior direction. In the mandible, transversal and skeletal changes are less dramatic. Posteriorly, changes occur in late childhood with anteroposterior, transverse, and vertical growth. Rotational growth also occurs causing vertical alterations. The anterior mandible however seems to have smaller alveolar growth. Patients with severe hypodontia, the anterior mandible may be the most suitable site of implant placement.
Timing of dental implant placement seems to be safest during declining adolescent growth curve or near adulthood. Other aspects to consider include individual status of existing dentition, functional status, phonetics, and esthetics.
Survival rates show higher for mandibular (91-92%) vs. maxilla (71-86%). Anterior maxillary implants were 2.8 times greater chance to fail than those placed in the anterior mandible.
Conclusion: Implant location, sex of patient, and skeletal maturation level are the most important factors in the final decision of when to place implants. It is still recommended to wait for the completion of dental and skeletal growth except for severe cases of ectodermal dysplasia.
Topic: Implant placement in young individuals
Title: Facial development, continuous tooth eruption, and mesial drift as compromising factors for implant placement
Source: Int J Oral Maxillofac Implants 2006 Nov-Dec;21(6):867-78
DOI: None
Type: Review
Keywords: alveolar process, dental esthetics, dental implants, facial growth, jawbone, orthodontics, puberty
Purpose: Osseointergrated implants do not follow changes in the alveolar processes caused by displacement, remodeling, mesial drift of the jawbones, and continues eruption of adjacent teeth. This results in a significant risk of a less favorable esthetic and/or functional outcome. This review aims to explain these phenomena and provides some guidelines for timely implant placement.
Discussion: The replacement of teeth lost in children can be an important indication for early implant therapy. Osseointergrated dental implants behave like ankylosed teeth. Skeletal growth in the close vicinity around implants are slowed down, whereas they continue at normal pace elsewhere, leading to an observation of bony defects, occlusal scheme dysfunctions, and adjacent tooth complications.
Facial growth of the child and even of the adolescent, as well as the continuous eruption of the adjacent anterior teeth, create significant risk of a less favorable esthetic and/or functional outcome.
Jaw bone growth: Both the mandible and the axilla follow a distinct chronology: growth is first completed in the transversal plane, then in the sagittal plane, and finally, only at a later stage, in the coronal plane. The growth of the mandible is closely associated with growth in stature, whereas growth for the maxilla is more associated with growth of the cranial structures.
Maxilla: intercanine arch width increases minimally after 10 years (0.9mm average), sagittal growth of maxilla typically is resorptive therefore implants placed in the anterior maxilla can come across the complication of buccal plate resorption and implant dehiscence, vertical growth of maxilla persists to 17-18 years of age in females, perhaps longer for males therefore until the age of 18 (approx.) there may be vertical plane issues.
Mandible: transverse growth completes early in anterior region whereas continue substantially in premolar and molar region, therefore if implants are placed in that region before growth cease implants could result lingually, vertical growth is substantial for mandible and is therefore can be affected by presence of dental implants. For patients with a normal facial profile, the placement of an implant should be postponed until skeletal growth is complete. For patients with a short or long face type, further growth, especially the continuous eruption of adjacent teeth, creates a serious risk even after the age of 25 years.
Conclusion: In order to determine proper timing for implant placement in adolescents/young adults it was suggested to examine:
- Continuous eruption should be considered and evaluated not only in adolescences but also adulthood when implant therapy is treatment planned.
- Lack of proper occlusion due to jaw growth may compromise oral rehabilitation using implant supported protheses and unesthetic situations can occur, especially in the anterior region.
- timeframe for the development of the alveolar process can vary widely, especially in the case of long or short facial types.
- For patients with a normal facial profile, the placement of an implant should be postponed until growth is complete.
- For patients with a short or long face type, further growth, especially the continuous eruption of adjacent teeth, creates a serious risk even after the age of 20 years.
Topic: Treatment planning- Skeletal growth
Authors: Fudalej P, Kokich V, Leroux B
Title: Determining the cessation of vertical growth of the craniofacial structures to facilitate placement of single-tooth implants.
Source: Am J Orthod Dentofacial Orthop. 2007 Apr; 131 (4 Suppl):S59-67
DOI:
Type: Retrospective study
Keywords: dental implant; cephalograms; puberty; facial skeleton growth
Purpose: To determine and quantify the amount of vertical growth of the facial skeleton and the amount of eruption of the central incisors and the maxillary first molars after puberty
Methods:
- 301 of 645 subjects selected: each subject had pretreatment, end of treatment, at least 10 year post treatment
- Patients divided into 2 samples: males (142) and females (159)
- Two or 3 lateral cephalograms taken at pretreatment, posttreatment, and 10 years post retention
- landmarks were identified on the lateral ceph and two planes were created: palatal and mandibular
- total change in anterior face height was assessed (distance from nasion to menton) along with the amount of eruption between maxillary and mandibular central incisors and molars (distance from incisal edge to palatal plane or mandibular plane)
- chi square test performed to evaluate differences in distribution of Angle classification and extraction treatment alternative
- Linear regression models were used to determine changes in the parameters with increasing age
Results:
- In males, anterior facial height increased 9.4mm during the observation time
- 50% of the increase occurred before age 15
- In females, anterior facial height increased 4.3mm during the observation time
- 40% of the increase occurred before age 15
- For both sexes, 60-70% of anterior facial height increase occurred in the lower anterior facial height
- In males, the total eruption of maxillary incisors was 2.0mm
- 50% of the eruption occurred before age 15
- In males, the total eruption of the mandibular incisors was 5.0mm
- 46% of the eruption occurred before age 15
- In females, the total eruption of the maxillary incisors was 2.7mm
- 44% of the eruption occurred before age 15
- In females, the total eruption of the mandibular incisors was 2.4mm
- 33% of the eruption occurred before age 15
- In males, the total eruption of maxillary molars was 4.0mm
- 5mm of the eruption occurred before age 15
- In females, the total eruption of the maxillary molars was 1.7mm
- 65% of the eruption occurred before age 15
Conlusion:
- The growth of the facial skeleton is a continuous process which increases around puberty but then decreases with time – especially after 20 years old
- increase in anterior facial height due to vertical growth is rapid during the teens
- there is a difference in the amount of growth between the sexes during the second decade of life
- the rate of eruption of the maxillary central incisors in females is greater than in males.
Topic: Implant age
Author: Oesterle L., Cronin R.
Title: Adult Growth, Aging, and the Single-Tooth Implant
Source: Int J Oral Maxillofac Implants 2000 Mar-Apr;15(2):252-260.
DOI:
Type: Discussion
Keywords: adult growth, aging, single tooth implant
Purpose: Review the research on changes due to growth and aging in the adult face, arches, and dentition and relate these to the effect of those changes on a single tooth implant prosthesis.
Discussion:
- Soft Tissue Changes: Cranium is nearly the young adult size by 7 or 8 years. Most of the changes that occur in the face happen due to the downward and forward growth of mandible relative to the maxilla as well as the increased size of the frontal sinuses and nose. The face will continue to grow throughout adulthood due to age (sagging and wrinkling), physical, and environmental (smoking, sun exposure) factors. For soft tissue the ears grow, eyebrows become lower and more prominent, and the nose becomes longer and more angulated. The upper and lower lips with increase in length, decreasing maxillary incisor exposure, increasing mandibular incisor exposure and decreasing vermillion lip exposure.
- Bony Changes: Bony changes associated with soft tissue changes are due to remodeling because sutures are fused earlier in life. There is growth in the anterior and posterior direction with most growth occurring in the lower face. Males show a greater increase in posterior height than females, who have equal growth posterior and anteriorly. Tooth loss will affect facial growth, but only with multiple teeth. The chin in males grows more horizontally, while in females it grows more vertically. No changes seen in glenoid fossa.
- Dentition Changes Maxillary incisors upright themselves pushing their roots more labially by around 2-3 degrees. Maxillary molars upright, as do mandibular molars in males but show mesial tipping in females. The arch depth and shape will decrease over time about 0.6-1.6mm causing crowding and an increase in the Curve of Spee forming a squarer arch shape.
- Implant Consideration Males should be considered questionable implant candidates until the age of 25, and females should be considered questionable until at least age 17 keeping in mind the potential for growth during childbearing years long term. The movement of maxillary anterior teeth could show a change in implant position compared to natural teeth after 2 decades or more. The mandible will show the greatest change in implant position compared to natural teeth due to movement of the teeth in a protrusive and vertical direction as well as crowding that occurs over time. The vertical growth seen in natural teeth in the posterior could lead to an implant crown being out of occlusion after several decades but wear of natural dentition could reverse these effects and possibly damage the implant itself.
Conclusion: Effects of growth and aging are normally subtle and occur very slowly but can be substantial in highly growing patients. Pretreatment counseling may be needed to explain implant crown modifications or replacements after 2 or more decades due to these changes in growth.
Topic:Patient age
Title: Effect of Age on Single Implant Submersion Rate in the Central Maxillary Incisor Region: A Long-Term Retrospective Study
Source: Clinical Implant Dentistry and Related Research, Volume 17, Number 3, 2015
DOI: 10.1111/cid.12131
Type: Retrospective Study
Keywords: age, dental implants, long term, submersion rate
Purpose: to evaluate the effect of age on the mean submersion rate of single dental implant, replacing a central maxillary incisor, placed after growth has ceased, as compared with the adjacent incisor natural tooth.
Methods: the retrospective study was conducted on patient’s files who received a single implant to replace a missing maxillary anterior tooth from 1992 to 2008. The study included 35 patients with a mean age of 29 years at implant placement, 14 of which were females. Criteria of patient selection:
- Missing maxillary central incisor between two natural teeth
- With clinical and radiographic follow-up of at least 3 years.
Most of implants were placed by one operator whereas 10 implant placements were placed by various others. Mean follow up time was 7.5 years and patients were divided into two groups according to the age at time of implant placement: <30 and >30 years old. Photos from the last follow-up were used to assess the change in the vertical dimension between the incisal edges of the implant supported crown of the missing central and the adjacent natural central incisor, considering that the restoration was performed at the same incisal level. Images were digitally analyzed using Image J software and due to the lack of scaling and uniformity of the photos, the mean submersion rate was defined in terms of percent of crown occlusal-gingival length per year.
Results: Implant submersion rates were o.48 for males and 0.82 for females. Results were not SSD (p=.087).
Discussion: The results of the present research suggest that whereas implant submersion continues throughout adult life its mean rate varies with age. It is evident that this phenomenon is much more conspicuous during the second and third decades of life as compared with the fourth and fifth.
Conclusion: The continuous submersion of the implant crown would result in pocketing and inflammation due to the continuous eruption of the adjacent teeth leading to shifting of the bacterial population and dominance of anaerobic bacteria. Changing the implant crown may not be biological efficient but will be esthetically important. Free gingival grafts to correct the problem can be beneficial.
Topic: Age at placement
Title: Thematic Abstract Review: Implants and the Spectrum of Aging.
Source: Int J Oral Maxillofac Implants 2017 Sep/Oct;32(5):965-968
DOI: –
Type: Review
- Oral health care needs of the elderly, continue to be seen as being largely unmet.
- No consistent definition of “elderly” exists, but 65 years of age is a common cutoff in the literature
- Subclassifying into three groups: functionally independent, functionally dependent, and institutionalized.
- With advanced age, ability to perform tasks of daily living declines. Need for assistance rises. Within a dental context, poor oral health status due to limited ability to perform oral self-care or to access professional dental services.
- The increasing need to rely on substitute decision makers and restricted wheelchair access are also factors that may become barriers to the access of qualified dental care services.
- Mean age of patients receiving implants appears to be rising. Researchers found that the overall age- at-treatment distribution is shifting to the right. Elderly patients (defined in this study as older than 70 years of age) constituted 7.7% of the treated patients in 2002 to 2004 time period, 11.0% of the treated patients in the 2008 to 2010 time period, and 21.0% of the treated patients in 2014.
- Compared with an average person, bone quality and quantity are likely compromised in the elderly, while implants and prostheses in elderly people are likely subjected to increased plaque burden but decreased masticatory forces.
- Systematic review (Srinivasan et al): The elderly cohort was defined as ≥ 65 years of age. After a thorough search, 11 studies were included in the analysis. The mean age of patients in most studies was 65 to 70 years. Only two studies focused on those older than 80 years of age. The random effects model revealed that 1-year, 3-year, 5-year, and 10-year postloading implant survival rates were 97.7%, 96.3%, 96.2%, and 91.2%, respectfully.
- Hoeksema et al: elderly patients with implant-supported overdentures and those with remaining teeth performed better on a range of survey parameters than completely edentulous elderly patients with conventional prostheses.
- Removable implant-supported restorations need to be designed so that retention can be lessened to account for decreased hand strength and dexterity.
- Fixed implant-supported restorations need to be designed so that, if necessary, they can be converted to removable alternatives later in life.
- A recent randomized controlled trial (RCT) (Merz et al) examined attitudes toward dental implant treatment in a geriatric institutionalized: Overall, approximately 20% to 25% expressed willingness to receive implants. Not ready to undergo dental implant treatment, cost (78.4%) and fear of surgery (43.1%) were found to be the primary reasons for their decision.
- Research focusing on dental implant care in the elderly is challenging, especially in the very elderly. Enrollment in intervention studies can be complicated by significant health compromise. Duration of follow-up can be significantly limited by a high dropout rate due to loss of independence and mobility, heath decline, and mortality.
- The overall impression is that the success of implant therapy per se is unaffected by aging and that the elderly can and do greatly benefit from the support and retention provided by the osseointegrated implants. However, access to qualified dental care providers who are experienced in delivering dental care services -including dental implant services- to the elderly cohort may be limited.
- Educational and research efforts should focus on reducing barriers to dental treatment in this vulnerable population group. The elderly with functional, cognitive, and health compromises are particularly likely to benefit from effective treatment approaches that are expedited, minimally invasive, and economic.
Topic: AGE AT PLACEMENT
Title: Influence of Age on Clinical Performance of Mandibular Two‐Implant Overdentures: A 10‐Year Prospective Comparative Study
Source: Clin Implant Dent Relat Res. 2016 Aug;18(4):745-51.
DOI: doi.org/10.1111/cid.12351
Type:10 yr prospective comparative study
Purpose: The aim of this prospective comparative study was to assess whether age has influence on peri‐implant health in patients treated with mandibular two‐implant overdentures during a 10‐year evaluation perio
Methods: A prospective study was carried out with two groups of edentulous patients, viz a younger (n = 52; mean age 45 years, 35–50 years) and an older (n = 53; mean age 68 years, 60–80 years) group. In all patients, two dental implants were placed in the interforaminal region of the mandible and after a 3‐month healing period overdentures were fabricated. Clinical and radiographic parameters were evaluated immediately after completion of the prosthetic treatment, and after 1, 5 and 10 years. Implant loss, plaque index, gingival index, bleeding index, and probing depth were assessed as clinical parameters. Peri‐implant bone loss was assessed on dental radiographs made with a standardized long‐cone technique with a direction device.
Results: Implant survival after 10 years was 97.1% and 93.4% in the younger and older group, respectively. Ten‐year scores of plaque, gingiva, and bleeding were between 0 and 1 for both groups (possible scores 0–3), and mean probing depth was 3 mm in both groups. Mean peri‐implant bone loss after 10 years was 1.2 and 1.4 mm in the younger and older patients, respectively. No significant differences were observed between the groups.
Discussion: Clinical performance of mandibular two‐implant overdentures is equally successful in younger and older patients.
Topic: Evaluation of dental implants in an aged population.
Title: Dental Implants in an Aged Population: Evaluation of Periodontal Health, Bone Loss, Implant Survival, and Quality of Life.
Source: Clin Implant Dent Relat Res. 2015
DOI: https://onlinelibrary.wiley.com/doi/epdf/10.1111/cid.12340
Type: Study
Keywords: bone changes; elderly patients; implant survival; medications; periodontal health; quality of life
Purpose: To evaluate aged partially and fully edentulous patients who received dental implants and were maintained over time.
Methods:
- Patients from 66 and 93 years of age.
- Bone grafting or sinus lifting were not performed.
- 15 males from 78 and 89 years old.
- 16 females from 66 to 93 years old.
- All implants were manufactured by Nobel Biocare.
- Thirty implants were placed using a flapless approach.
- 35 placed with a flapped two-stage approach.
- 19 were placed with a flapless immediate implant protocol.
- 54 implants were placed in maxilla with a loss of two.
- 30 implants were in mandibles with loss of two.
- Of the 31 patients, 3 have deceased, 2 are in living nursing homes, and 2 patients could not be located.
- 25 patients were evaluated in this study.
Radiographic Evaluation.
- The radiographic measurements were taken at the second stage appointment, prior to implant restoration and at the longest follow-up evaluation.
- Non-standardized parallel long cone periapical radiograph was taken.
- Mesial and distal bone levels were measured using Image J.
Clinical Evaluation.
- Periodontal evaluation was based on Periodontal Disease Index
- For natural teeth, probing depth, plaque, bleeding on probing, and mobility were evaluated.
- Blinded 7 question quality of life questionnaire was sent to all patients.
Statistical Methods.
- Descriptive statistics were used to compare changes in clinical measurements.
- Kaplan–Meier survival probabilities were used to determine the implant survival.
Results:
- The mean probing depth for 25 examined were statistically insignificant.
- Comparison of measured bone levels between a previously reported control group was made with the aged group for implant length and width, crestal bone levels at implant insertion, and longest follow-up and change in bone height.
- Changes between control and aged groups were significant only for implant diameter .
- Most patients classified themselves as having a good quality of life with minimal distress from eating, relaxing, and socially engaging.
- 15 patients did not perceive a change in quality of life.
- 8 had improvement oral health.
- 8 out of 33 of the patients were lost to follow-up.
- 6 to 7-year follow-up the implant survival rate was 94.6%. (Assumes patients lost to follow-up have not lost implants).
Discussion:
- Implants placed in an aged population have excellent clinical outcomes in terms of implant survival and maintenance of periodontal health with minimal long-term loss of interproximal bone levels.
- With careful diagnosis and treatment planning, aged patients are excellent candidates for dental implants.
- Caution must be exercised, as many of these patients are taking multiple medications.
Topic: Implants in aged patients
Title: Effect of advanced age and/or systemic medical conditions on dental implant survival: A systematic review and meta‐analysis
Source: Clin Oral Implants Res. 2018 Oct;29 suppl 16:311-330.
Background: In the scope of this review, geriatric patients were defined as patients with an age of 75 years and above.
Objective: The aim of this systematic review was to screen and pool the available evidence to establish: 1. The dental implant survival rate in geriatric patients. 2. The potential impacts of the most common systemic medical conditions (WHO, 2015) and their treatments on implant survival.
The focused question set for this systematic review was “In patients undergoing dental implant therapy, what is the effect of advanced age (≥75 years) and/or common systemic medical conditions on the implant survival, biological complication, and technical complication rates?” Dental implants that satisfied inclusion criteria were included in the first part of this systematic review, which analyzed implant survival.
Therefore, outcomes in healthy aged people were also sought. Exclusion criteria:
- Age <75
- years One‐piece implants, Zygomatic implants, and pterygoid implants
- Post-loading follow‐up <12 months
- Narrow diameter implants or mini dental implants (implants with diameter <3 mm)
- Implants with turned or machined surface
For the second part of this search, no age limit was applied, as a preliminary screening of the literature did not identify any studies in relation to the most common medical conditions in the elderly (WHO, 2015) if the exclusion criteria included those aged 75 years or older.
Articles sources were MEDLINE (PubMed), online internet search engines (e.g., Google and Yahoo), research community websites on the internet, reference cross‐checks, personal communications, and hand searches. Hand searches in dental journals were only performed for records not available electronically or without an electronic abstract
Results: 46 relevant articles were shortlisted for inclusion in the review. After subsequent hand searches, reference cross‐checks, and information from other sources and authors, an additional 16 articles were identified.
First part: Patients who are 75 years and older showed high implant survival rates.
Second part: Medical conditions and their treatment:
Cardiovascular disease (including ischemic heart disease, stroke, hypertensive heart disease): Implant survival in relation to CVD or associated treatment was reported in two studies. In particular, one article reported a higher survival rate of implants in patients treated with antihypertensive therapy. In contrast, a second article did not find an influence of hypertensive heart disease on implant survival.
Cancer
Radiotherapy:
Seventeen studies were identified which met the inclusion and exclusion criteria, most investigators reported a time lapse between radiotherapy and implant placement of more than 12 months; however, some utilized a shorter delay.
Antiresorptive therapy:
Antiresorptive therapy (ART) may be associated with medication‐related osteonecrosis of the jaw (MRONJ), however, in studies of osteoporotic patients managed with ART, reported implant survival rates were predominately high. The prevalence of MRONJ in these patient cohorts was rarely specified.
Diabetes mellitus
Calculated survival rates were reported to range from 86.3% (24‐month observation period) to 100% (12 months). Poor control (HbA1c ≥ 8.0%) may have an influence.
Neurocognitive impairment (unipolar depression, Alzheimer’s disease and other dementias, and Parkinson’s disease)
One study reported higher implant failure rates in patients taking selective serotonin reuptake inhibitors for depression compared to nonusers of SSRIs, Case reports and case series with a limited number of participants reported on patients with Parkinson’s disease with calculated survival rates ranging between 82.1% and 100%.
No articles reporting on implant survival in patients with Osteoarthritis, Cirrhosis of the liver, Respiratory diseases (chronic obstructive pulmonary disease COPD and lower respiratory infections).
Discussion:
This review identified high implant survival rates in geriatric patients aged 75 years and older. Cardiovascular disease:
the current review identified one study that reported the positive impact of antihypertensive drugs on implant survival (Wu et al., 2016). The authors hypothesize that this may be related to the positive effect of such drugs including beta‐blockers, thiazide diuretics, ACE inhibitors, and ARBs on bone metabolism.
Radiotherapy:
The use of head and neck radiotherapy has been associated with a reduced survival rate of implants Antiresorptive therapy and osteoporosis
Dental implant treatment is often contraindicated in these patients because of the strongly increased risk of MRONJ Diabetes:
HbA1c levels above 8% may result in reduced implant survival compared to lower levels.
Conclusion: Implant prostheses in geriatric subjects are a predictable treatment option with a very high rate of implant survival. The functional and psychosocial benefits of such intervention should outweigh the associated risks to common medical conditions.
Book References:
Medical History: medical conditions + drugs that may affect implant and surgical outcome; Risk factors
- Misch and Resnik. Medical Evaluation of the Dental Implant Patient (CH 20). pp 406-420. Contemporary Implant Dentistry, Misch, C.E., 3rd Edition, 2008, Mosby Year Book.
- Rose L and Mealey B. Implant complications associated with systemic disorders and medications. (CH 2) pp 9-45.
